Population: Pregnant women with gestational diabetes.
Organizations
 ACOG 2018, SMFM 2018, NICE 2015, ADA 2023
ACOG 2018, SMFM 2018, NICE 2015, ADA 2023
Recommendations
Management
–Employ nutrition therapy and exercise.
–Counsel those with estimated fetal weight of 4500 g or more regarding the option of scheduled cesarean delivery vs. vaginal trial of labor.
–Instruct patients to follow fasting and 1-h postprandial glucose levels. Target fasting blood glucose of 95 mg/dL and 1-h postprandial of 140 mg/dL or 2-h postprandial of 120 mg/dL.
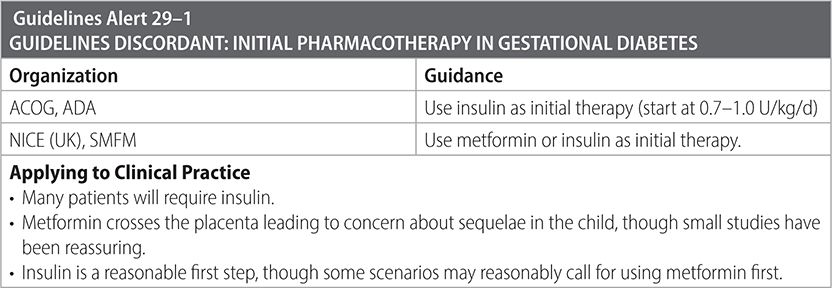
–Use pharmacotherapy to achieve blood glucose goals when lifestyle modification is unsuccessful (see Guidelines Discordant table below).
–Start low-dose aspirin 100–150 mg/day (162 mg “may be acceptable”) beginning between 12 and 16 wk to lower risk of preeclampsia in every pregnant person with type 1 or type 2 diabetes.
–Unless otherwise indicated, do not induce those with well-controlled A1 GDM before 39 wk. Expectant management until 40-6/7 wk is appropriate.
–For women with A2GDM, delivery is recommended at 39-0/7 to 39-6/7 wk of gestation.
Surveillance
–Start antepartum fetal testing at 32-wk gestational age in those requiring medication or under poor control and without other comorbidities. Consider starting surveillance earlier if other comorbidities are present. For those with A1 GDM and no comorbidities, antepartum testing may not be necessary.
–Screen all women with GDM with a 75-g 2-h GTT 4–12 wk after delivery. Continue some form of screening q 1–3 y lifelong.
–Advise postpartum weight loss to reduce future risk of DM2.

Sources
–ACOG Practice Bulletin No. 190: Gestational Diabetes Mellitus. Obstet Gynecol. 2018;131(2):e49-e64. https://www.scribd.com/document/371228843/190-Gestational-Diabetes-Mellitus-Agog
–NICE. Diabetes in pregnancy: management from preconception to the postnatal period (NG3). 2015.
–Am J Obstet Gynecol. 2018;218(5):B2-B4.
–Diabetes Care. December 2023;46(Suppl.1):S254-S266.