Population: Adults with AF.
Organizations
 NICE 2021, AHA/ACC/HRS 2019, ESC 2018, ACCP 2018
NICE 2021, AHA/ACC/HRS 2019, ESC 2018, ACCP 2018
Recommendations
–If hemodynamically unstable, use electric or pharmacologic cardioversion urgently. Anticoagulate (heparin or dabigatran/argatroban) as soon as possible and continue for at least 4 wk.
–If hemodynamically stable, obtain rate control. Pursue rhythm control only if symptoms persist after rate control or rate control is unsuccessful.
Management of Rate
–Acutely slow the rate to <110 bpm with IV beta-blocker or calcium channel blocker (Tables 19–1 to 19–4).
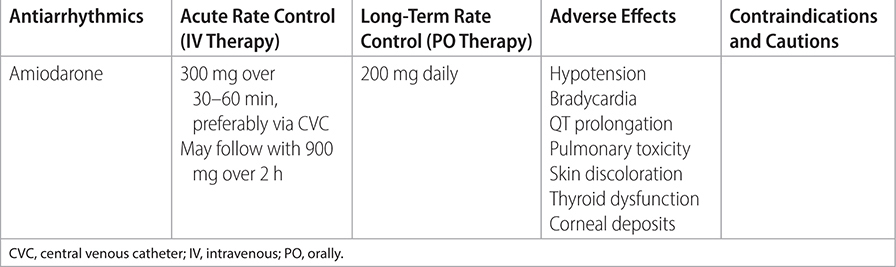
–For chronic rate control, use beta-blocker or nondihydropyridine calcium channel in both persistent and paroxysmal AF. If unsuccessful or contraindicated, consider amiodarone (ACC/AHA) or digoxin (ESC).
–If asymptomatic and LVEF is preserved, titrate medication to a resting heart rate <110.
–If symptomatic at HR <110, titrate medication to a resting heart rate <80.
–If rate and/or rhythm control strategies fail, consider AV nodal ablation and pacemaker placement.
Management of Rhythm
–For chronic rhythm control, use dronedarone, flecainide, propafenone, or sotalol.
–Avoid amiodarone for long-term antiarrhythmic unless concomitant heart failure (HF), given considerable side effect profile.
–Avoid flecainide or propafenone if evidence of ischemic or structural heart disease.
TABLE 19–1 RATE CONTROL IN ATRIAL FIBRILLATION: BETA-BLOCKERS
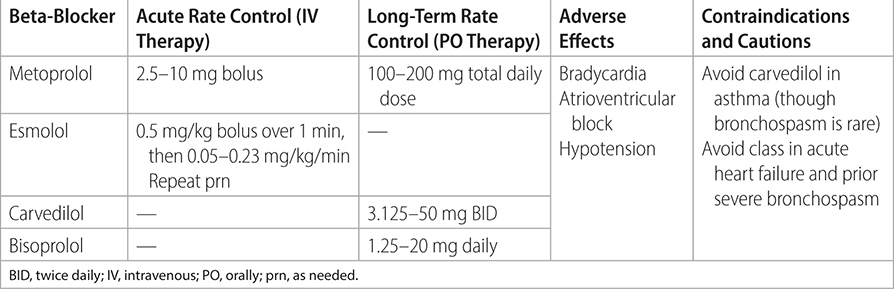
TABLE 19–2 RATE CONTROL IN ATRIAL FIBRILLATION: CALCIUM CHANNEL BLOCKERS
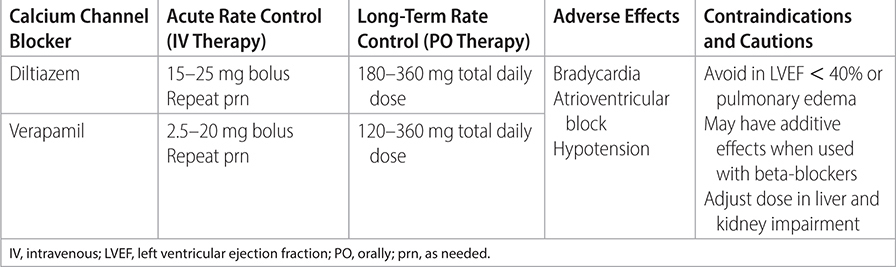
TABLE 19–3 RATE CONTROL IN ATRIAL FIBRILLATION: CARDIAC GLYCOSIDES
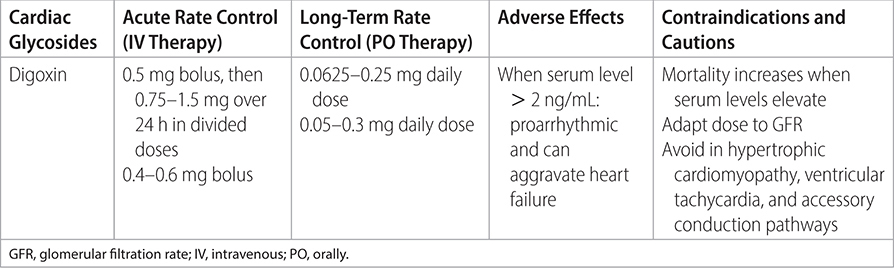
TABLE 19–4 RATE CONTROL IN ATRIAL FIBRILLATION: ANTIARRHYTHMICS
–Consider catheter ablation of AF as initial rhythm-control strategy,1 or after failure of an antiarrhythmic medication. Only offer ablation if patients can be anticoagulated for at least 8 wk after procedure.
–Consider AF catheter ablation in selected patients with symptomatic AF and HF with reduced left ventricular (LV) ejection fraction (HFrEF), as it may lower mortality rate and reduce hospitalization for HF.
–Consider antiarrhythmic drug treatment for 3 mo after left atrial ablation.
Practice Pearls
• AF guidelines apply to patients with atrial flutter as well.
• Risk factors for AF include age > 60, CKD, COPD, valvular heart disease, OSA, tobacco use, MI, HF, hyperthyroidism, obesity, HTN, and heavy alcohol use.
• ACC/AHA definitions of AF:
- Paroxysmal: Terminates within 7 d of onset.
- Persistent: Sustained continuously >7 d.
- Long-standing persistent: Sustained continuously >12 mo.
- Permanent: Declared once patient and physician decide to stop trying to restore sinus rhythm.
- Nonvalvular: Mitral stenosis, prosthetic valve, or mitral valve repair absent.
• Expected ventricular heart rate (HR) in untreated AF is between 110 and 210 beats/min.
- If HR < 110 beats/min, atrioventricular (AV) node disease present.
- If HR > 220 beats/min, preexcitation syndrome (WPW) present.
• Holter monitor best measures the adequacy of the chronic HR control. In acute medical conditions when the patient has noncardiac illness (ie, pneumonia), the resting HR may be allowed to increase to simulate physiologic demands (mimic HR if sinus rhythm was present). (ESC recommends HR target <110 beats/min; CCS recommends <100 beats/min; ACCF/AHA/HRS recommends HR target <110 beats/min only if EF > 40%.)
• Choosing Wisely: American Society of Echocardiography (2013) recommends against transesophageal echocardiography to detect cardiac sources of embolization if a source has been identified and patient management will not change. (http://www.choosingwisely.org/sourcessocieties/american-society-of-echocardiography/)
• Various studies (AFFIRM, RACE, PIAF, STAF, etc.) have failed to show quality of life difference for rhythm control vs. rate control. Rhythm control is more likely to be effective in symptomatic patients who are younger with minimal heart disease, few comorbid conditions, and recent onset of AF.
Sources
–JACC. 2014;64(21):2246-2280. http://www.onlinejacc.org/content/64/21/2246
–Eur Heart J. 2016;37:2893-2962.
–Eur Heart J. 2018;39(16):1330-1393. https://academic.oup.com/eurheartj/article/39/16/1330/4942493
–2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS. Guideline for the Management of Patients with Atrial Fibrillation.
Population: Adults with AF and heart failure with reduced ejection fraction (HFrEF).
Organizations
 AHA/ACC/HRS 2014, ESC 2016, NICE 2021
AHA/ACC/HRS 2014, ESC 2016, NICE 2021
Recommendations
–Acutely, avoid calcium channel blockers in patients with LV ejection fraction <40%. Use only beta-blockers and digoxin as rate controllers in HFrEF because of the negative inotropic potential of verapamil and diltiazem.
–Long term, choose amiodarone rather than other antiarrhythmics in patients with HF. Otherwise do not choose amiodarone for AF without HFrEF for long-term antiarrhythmic because of side-effect profile.
–Consider catheter ablation to restore LV function in AF patients with HFrEF, though further data are still needed.
Sources
–JACC. 2014;64(21):2246-2280. http://www.onlinejacc.org/content/64/21/2246
–Eur Heart J. 2016;37:2893-2962.
–NICE guideline 196. Atrial fibrillation: diagnosis and management. 2021.
Population: Adults with AF and heart failure with preserved ejection fraction (HFpEF).
Organizations
 AHA/ACC/HRS 2014, ESC 2016
AHA/ACC/HRS 2014, ESC 2016
Recommendations
–It may be difficult to separate symptoms that are due to HF from those due to AF.
–Focus on the control of fluid balance and concomitant conditions such as hypertension and myocardial ischemia.
Sources
–JACC. 2014;64(21):2246-2280. http://www.onlinejacc.org/content/64/21/2246
– Eur Heart J. 2016;37:2893-2962.