Population: Adults with osteoarthritis.
Organizations
 ACR 2019, NICE 2022
ACR 2019, NICE 2022
Recommendations
Evaluation
–Diagnose OA clinically without imaging for patients who meet all of the following:
• Age ≥45 y.
• Have pain related to activity.
• Have no morning stiffness or morning stiffness lasts <30 min.
–Order imaging to diagnose OA if there are atypical features that suggest potential alternative diagnoses.
Management
–Strongly recommend individualized therapeutic exercises (eg, strength, aerobic, aquatic) for all people with OA.
–Recommend supervised exercise with physical therapy and/or occupational therapy over unsupervised exercise as this improves outcomes.
–Strongly encourage weight loss for overweight and obese patients to improve quality of life and physical function, as well as reduce pain, for all joint-related OA and particularly for lower extremity OA. Provide information regarding self-efficacy and self-management programs.
–Recommend the use of walking devices (such as canes) for lower extremity OA or hand orthoses for CMC OA if it is likely to improve function and reduce pain.
–Recommend tai chi for lower extremity OA.
–Consider balance exercises, yoga, cognitive behavioral therapy, thermal interventions, and kinesiotaping (only hand or knee OA).
–Approach to medications:
• Offer topical NSAIDs for knee OA. Consider topical NSAIDs for other joints with OA.
• If topical NSAIDs are ineffective, treat with oral NSAIDs if not contraindicated at lowest effective dose. If taken consistently, offer gastroprotective treatment, such as a PPI.
• Consider duloxetine, topical capsaicin (except for hand OA), acetaminophen.
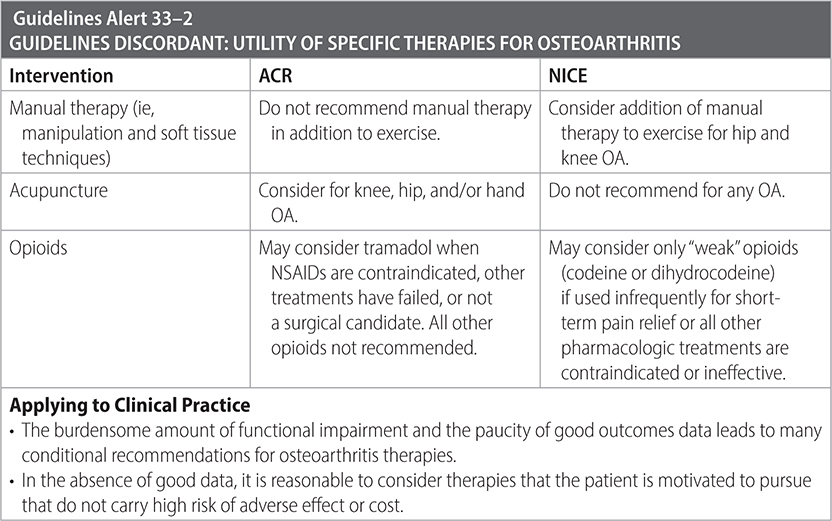
• Do not offer opioids other than tramadol (see “Guidelines Alert 33-2” table below for additional information), chondroitin sulfate, or glucosamine.
• Offer intra-articular steroid injections for short-term pain relief (2–10 wk) when other treatments are ineffective and/or to support therapeutic exercise.
• Do not offer dry needling, intra-articular hyaluronic acid injections, prolotherapy, platelet rich plasma (PRP), or stem cell therapies.
• Do not offer transcutaneous electrical nerve stimulation (TENS) treatment.
–Consider walking aids (such as canes) for lower extremity OA.
–Consider referral for joint surgery for people with OA and severe joint symptoms refractory to nonsurgical treatments.

Sources
–American College of Rheumatology. American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the hand, Hip, and Knee. 2019; rheumatology.org/Portals/o/Files/Osteoarthritis-Guideline
–BMJ. 2023;380:24.
Population: Adults with osteoarthritis of the hip.
Organizations
 AAOS 2017; NICE 2022
AAOS 2017; NICE 2022
Recommendations
–Screen for mental health disorders in patients with symptomatic hip OA who are undergoing total hip arthroplasty to improve outcomes.
–Unless contraindicated, offer NSAIDs for symptomatic hip OA for short-term pain relief.
–Offer intra-articular corticosteroid injections when other pharmacologic treatments are ineffective or contraindicated to reduce pain in the short term (2–10 wk) and improve function for symptomatic hip OA.
–Refer patients to physical therapy with mild-to-moderate symptoms of hip osteoarthritis to improve function and reduce pain.
–Consider referral for total hip arthroplasty for mild-to-moderate symptomatic hip osteoarthritis if pain is significantly impacting qualify of life and nonsurgical management is ineffective.
–Do not exclude patients from referral for total hip arthroplasty based on age, smoking, and obesity despite the possible association with increased risk of postoperative complications and poorer clinical outcomes.
–Recommend postoperative physical therapy to improve early function for those who have undergone total hip arthroplasty.
Practice Pearls
• Do not routinely order imaging studies to monitor disease progression of osteoarthritis, unless there has been an acute change in symptom quality or progression to evaluate for severity or rule out other diagnoses.
• The American College of Rheumatology and American Association of Hip and Knee Surgeons address the optimal timing for THA for symptomatic moderate-to-severe hip osteoarthritis. It is important to note that these guidelines are conditional and directed by the severity of OA with symptoms, rather than the severity of symptoms with OA in contrast to the aforementioned guidelines:
- Do not delay THA to pursue nonsurgical management.
- Delay THA to achieve nicotine reduction or cessation.
- Delay THA to achieve optimal DM control. The degree of DM control is not specified.
- Do not delay THA due to obesity alone, nor to achieve a specific BMI or weight target, though weight loss should be strongly encouraged.
- Do not delay THA due to deformity, bone loss, or presence of neuropathic joint.
Sources
–Ann Rheum Dis. 2017;76:1484-1494.
–BMJ. 2023;380:24.
–American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Hip Evidence-Based Clinical Practice Guideline. https://www.aaos.org/oahcpg. Published March 13, 2017.
–American College of Rheumatology and American Association of Hip and Knee Surgeons. Clinical Practice Guideline for the Optimal Timing of Elective Total Hip or Knee Arthroplasty for Patients with Symptomatic Moderate to Severe Osteoarthritis or Osteonecrosis Who Have Failed Nonoperative Therapy. Manuscript in preparation, 2023.
Population: Adults with osteoarthritis of the shoulder.
Organizations
 AAOS 2020, NICE 2022
AAOS 2020, NICE 2022
Recommendations
–Offer nonsurgical management prior to referring for surgical intervention, as patients with lower preoperative functioning experience higher postoperative functional improvement and older age is associated with lower revision rates.
–Refer for joint replacement if their OA-related pain is significantly interfering with quality of life and nonsurgical options are ineffective. The presence of night pain, pain flares, and joint instability symptoms are important indicators that surgery will likely be beneficial.
–Do not offer hyaluronic acid injections or injectable biologics (such as PRP or stem cells).
–Address concomitant depression in patients who are undergoing total shoulder arthroplasty (TSA) to improve postoperative outcomes.
–Encourage smoking reduction or cessation in patients who are undergoing TSA.
–May offer preoperative and postoperative physical therapy in select patients given potential benefit.
Practice Pearl
• Anatomic TSA demonstrates better function and pain relief in the short- and mid-term follow-up when compared to hemiarthroplasty. Anatomic TSA and reverse TSA may both be considered for patients with shoulder OSA in setting of excessive glenoid bone loss and/or rotator cuff dysfunction.
Sources
–AAOS. Management of Glenohumeral Joint Osteoarthritis, Evidence-Based Clinical Practice Guideline. The American Academy of Orthopaedic Surgeons Board of Directors. March 23, 2020.
–BMJ. 2023;380:24.
Population: Adults with osteoarthritis of the knee.
Organizations
 AAOS 2021, ACR 2018, ACR 2019
AAOS 2021, ACR 2018, ACR 2019
Recommendations
–Obtain knee x-ray as initial imaging for chronic knee pain, but do not order routinely.
–Use self-management and patient education programs to promote lifestyle habits aimed at preventing progression of knee OA.
–For overweight and obese patients with knee osteoarthritis, encourage sustained weight loss.
–Use exercise programs to improve both function and pain. Neuromuscular training programs can be used in combination with exercise programs.
–When not contraindicated, treat with topical/oral NSAIDs and acetamionphen to improve function and quality of life in those with knee OA.
–Offer intra-articular corticosteroid injections to provide short-term relief. Hyaluronic acid injections are not recommended.
–Recommend canes and tibiofemoral braces if likely to improve function and pain. Consider patellofemoral braces for patellofemoral OA if disease is significantly impacting ambulation and/or stability.
–Avoid arthroscopy with lavage and/or debridement for patients with primary diagnosis of knee OA.
–Consider arthroscopic partial meniscectomy to treat meniscal tears in patients with concomitant mild-to-moderate knee OA who have failed nonsurgical treatments.
Practice Pearls
• Physical therapy is superior to intra-articular corticosteroids in improving both pain and function in the long term, but they similarly improve short-term pain and function.
• ACR recommends against PRP for knee OA. AAOS recommends consideration of PRP to reduce pain and improve function.
• ACR recommends against the use of chondroitin, glucosamine, and vitamin D. AAOS recommends consideration of these agents due to potential to reduce pain based on limited evidence.
• The American College of Rheumatology and American Association of Hip and Knee Surgeons address the optimal timing for TKA for symptomatic moderate-to-severe knee osteoarthritis (final publication pending summer 2023):
- Do not delay TKA to pursue nonsurgical management.
- Delay TKA to achieve nicotine reduction or cessation.
- Delay TKA to achieve optimal DM control. The degree of DM control is not specified.
- Do not delay TKA due to obesity alone, nor to achieve a specific BMI or weight target, though weight loss should be strongly encouraged.
- Do not delay TKA due to deformity, bone loss or presence of neuropathic joint.
Sources
–American Academy of Orthopaedic Surgeons Management of Osteoarthritis of the Knee (Non-Arthroplasty) Evidence-Based Clinical Practice Guideline. https://www.aaos.org/oak3cpg. Published August 30, 2021.
–N Engl J Med. 2020;283:1420-1429.
–American College of Radiology. ACR Appropriateness Criteria® Chronic Knee Pain. https://www.acr.org/-/media/ACR/Files/Appropriateness-Criteria/RadiationDoseAssessmentIntro.pdf. Revised 2018.
–American College of Rheumatology. American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the hand, Hip, and Knee. 2019; rheumatology.org/Portals/o/Files/Osteoarthritis-Guideline
–American College of Rheumatology and American Association of Hip and Knee Surgeons. Clinical Practice Guideline for the Optimal Timing of Elective Total Hip or Knee Arthroplasty for Patients with Symptomatic Moderate to Severe Osteoarthritis or Osteonecrosis Who Have Failed Nonoperative Therapy. Manuscript in preparation, 2023.