Polymorphism in thiopurine methyltransferase (TPMT).
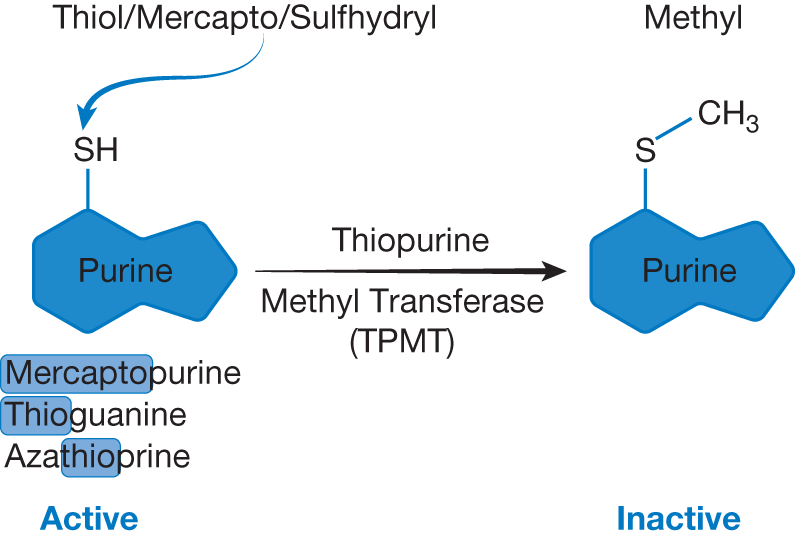
Substituting oxygen with sulfur has been one strategy to generate fake nucleic acids, which possess antineoplastic activity. These agents are called thiopurine or thiopyrimidine. TPMT is a cytoplasmic enzyme that methylates (i.e., adds CH3 group) aromatic compounds such as the thiopurine drugs 6-mercaptopurine (6-MP), 6-thioguanine, and azathioprine and inactivates them. The thiopurine drugs are used to treat acute lymphoblastic leukemia (ALL) or organ transplant patients.
TPMT gene is highly polymorphic. Checking the TPMT genetic polymorphism represents one of the first examples in which testing for a genetic variant of a drug-metabolizing enzyme has entered stand ard clinical practice. Genetic polymorphisms in TPMT result in trimodal distribution of TPMT activity in population: low (0.3%), intermediate (11.1%), and high (88.6%). Patients with low TPMT activity are at increased risk for thiopurine-induced myelotoxicity including severe neutropenia and thrombocytopenia as well as severe mucositis. The dose of thiopurine drugs in patients with low and intermediate TPMT activity needs to be reduced and complete blood count needs to be checked frequently.
6-MP and thioguanine are available as oral tablets or suspensions. 6-MP is also metabolized to inactive metabolite by xanthine oxidase; hence, 6-MP requires significant dose reductions (by 75%) if given concomitantly with xanthine oxidase inhibitors such as allopurinol or febuxostat that are commonly used for treatment/prevention of hyperuricemia.