- Verify the practitioner’s order.
- Gather and prepare the necessary equipment and supplies.
- Perform hand hygiene.4,5,6,7,8,9
- Confirm the patient’s identity using at least two patient identifiers.10
- Provide privacy.11,12,13,14
- Explain the procedure to the patient and family (if appropriate) according to their communication and learning needs to increase their understanding, allay their fears, and enhance cooperation.15 Inform the patient that the practitioner has ordered a right chest lead ECG, a procedure that involves placing electrodes on the arms, legs, and chest. Reassure the patient that the test is painless and takes only a few minutes, during which the patient will need to lie quietly on the back.
- Raise the patient’s bed to waist level before providing care to prevent caregiver back strain.16
- Have the patient lie supine in the center of the bed with the arms at the patient’s sides.1
- Raise the head of the bed as needed to promote patient comfort.17
- If the patient requires a position other than supine, document the position on the ECG tracing.2
- Perform hand hygiene.4,5,6,7,8,9
- Put on gloves, if needed, to comply with standard precautions.16,18,19
- Expose the patient’s arms, chest, and legs. Drape the patient appropriately with a bath blanket or sheet; drape a female patient’s chest until you apply the chest electrodes. Ensure that the patient’s arms and legs are relaxed to minimize muscle trembling, which can cause electrical interference.20
- Select electrode sites. Select flat, fleshy areas to place the limb lead electrodes. Avoid muscular and bony areas.2 If the patient has an amputated limb, choose a site on the residual limb.
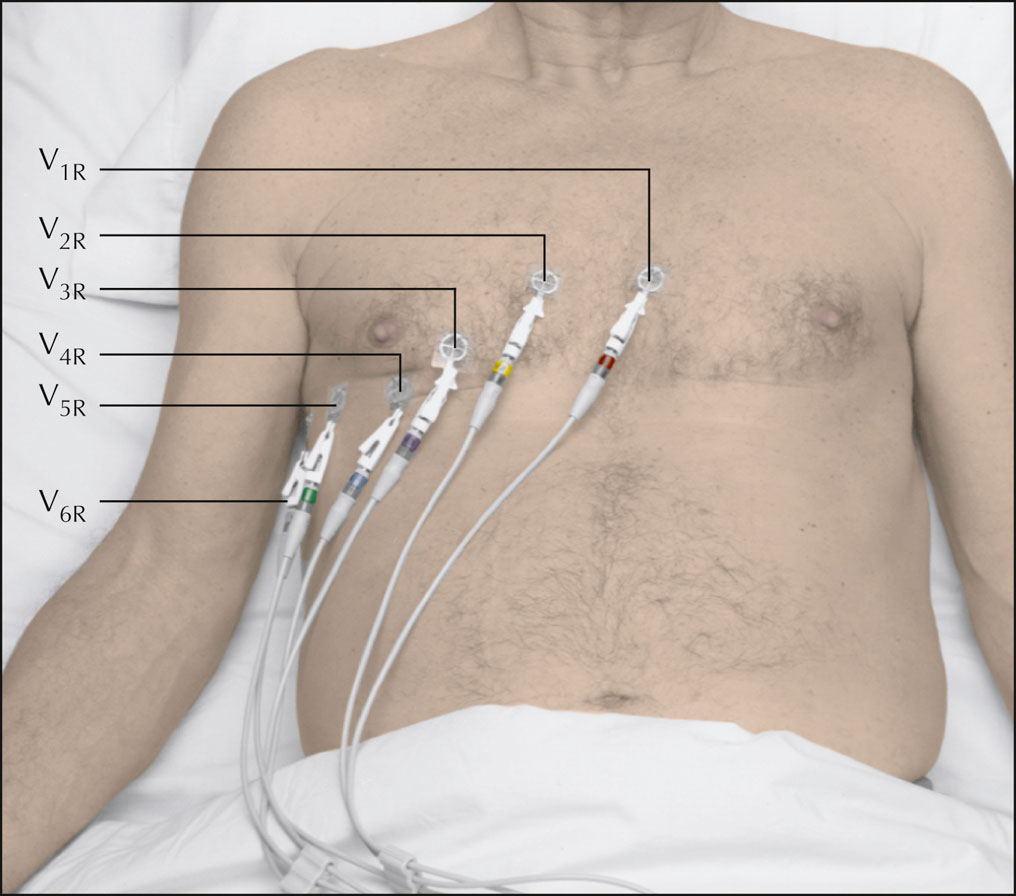
- Examine the patient’s chest to locate the correct sites for chest lead placement (as shown below). If the patient is female, you’ll place the electrodes under the breast tissue.2
- If an area is excessively hairy, clip the hair using a disposable-head clippers or single-patient-use scissors.2,20,21
- To enhance lead electrode contact and trace quality, prepare all the electrode sites by washing them with soap and water and drying them thoroughly; moist skin may prevent the electrodes from adhering.2 Rub the electrode sites briskly with a dry washcloth or gauze pad to remove dead skin cells and promote impulse transmission.2,20,21,22 If necessary, clean oily skin with an alcohol pad and allow it to dry.23,24
- Mark all the electrode sites with an indelible marker if serial ECGs are likely, to permit accurate comparison with future tracings.2
- Apply disposable pre-gelled electrodes to the prepared sites on the patient’s arms and legs, distal to the shoulders and hips, according to the manufacturer’s instructions.20 Position them in approximately the same location on each limb.2 To guarantee the best connection to the lead wire, position disposable pre-gelled electrodes on the legs with the lead connection pointing superiorly.
- Connect the lead wires to the electrodes. The lead wires are color-coded and lettered. Place the white, or right arm (RA), wire on the right arm; the black, or left arm (LA), wire on the left arm; the green, or right leg (RL), wire on the right leg; and the red, or left leg (LL), wire on the left leg.
- Apply a pre-gelled electrode at each electrode position on the patient’s chest.
- Use your fingers to feel between the patient’s ribs (the intercostal spaces). Start at the second intercostal space on the left (the notch felt at the top of the sternum, where the manubrium joins the body of the sternum). Count down two spaces to the fourth intercostal space at the left sternal border. Apply a disposable pre-gelled electrode to the site, and attach lead wire V1R to that electrode.2
- Move your fingers across the sternum to the fourth intercostal space at the right sternal border. Apply a disposable pre-gelled electrode to that site and attach lead V2R.2
- Move your finger down to the fifth intercostal space and over to the midclavicular line. Place a disposable pre-gelled electrode here and attach lead V4R. Apply a disposable pre-gelled electrode midway on this line from V2R and attach lead V3R.2
- Move your finger horizontally from V4R to the right midaxillary line. Apply an electrode to this site and attach lead V6R.2
- Move your fingers along the same horizontal line to the midpoint between V4R and V6R. This is the right anterior midaxillary line. Apply a disposable pre-gelled electrode to this site and attach lead V5R.2
- Ask the patient to breathe normally and to refrain from talking during the recording so that muscle movement won’t distort the tracing.
- Make sure that the paper speed is set at 25 mm/second and the amplitude at 1 mV/10 mm.10,11
- Press the AUTO or START key. The ECG machine will record all 12 leads automatically. Check your facility’s policy for the number of readings to obtain. (Some facilities require at least two ECGs so that one copy can be sent out for interpretation while the other remains at the bedside.)
- Observe the tracing quality. If any part of the waveform height extends beyond the paper when you record the ECG, adjust the normal standardization to half-standardization. Note this adjustment on the ECG strip, because this will need to be considered in interpreting the results.25
- When you’re finished recording the ECG, turn off the machine. If the ECG machine hasn’t already done so, label the ECG with the date and time as well as the patient’s name and identification number. Also label the tracing as RIGHT CHEST ECG to distinguish it from a standard 12-lead ECG.1 Make sure that the tracings are correctly labeled V1R through V6R.
- Remove the electrodes and discard them in the appropriate receptacle.
- Clean the patient’s skin with a gauze pad or moist cloth.
- Return the bed to the lowest position to prevent falls and maintain patients safety.26
- Remove and discard your gloves, if worn.16,19
- Perform hand hygiene.4,5,6,7,8,9
- Put on gloves, as needed.19
- Clean and disinfect the ECG equipment according to the manufacturer’s instructions to prevent the spread of infection.27,28 Prepare the equipment for future use.2
- Remove and discard your gloves, as needed.19
- Perform hand hygiene.4,5,6,7,8,9
- Place the ECG tracing in the patient’s medical record.
- Document the procedure.29,30,31,32