An arterial line provides access for invasive arterial pressure monitoring (e.g., continuous blood pressure monitoring) and can be used to obtain blood samples when frequent blood draws are indicated, including arterial blood gases.
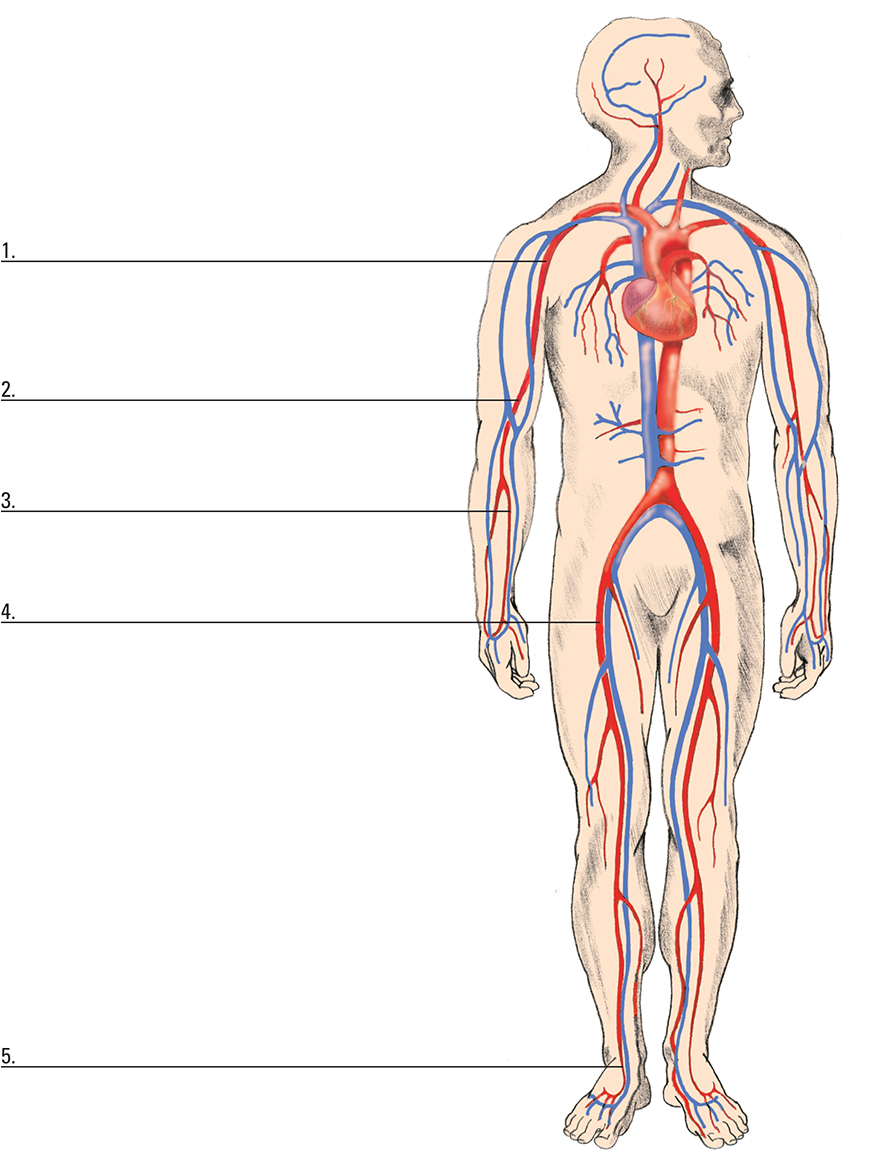
A closer look at arterial insertion sites
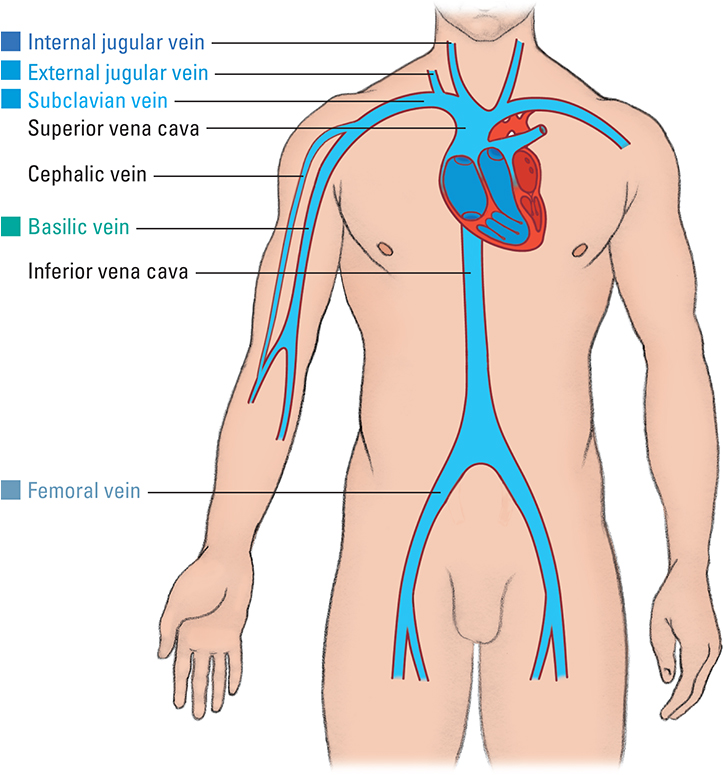
Typically, a standard 18G to 20G over-the-needle catheter is inserted into a peripheral artery, usually the radial, brachial, or femoral artery. The radial artery is the preferred site.
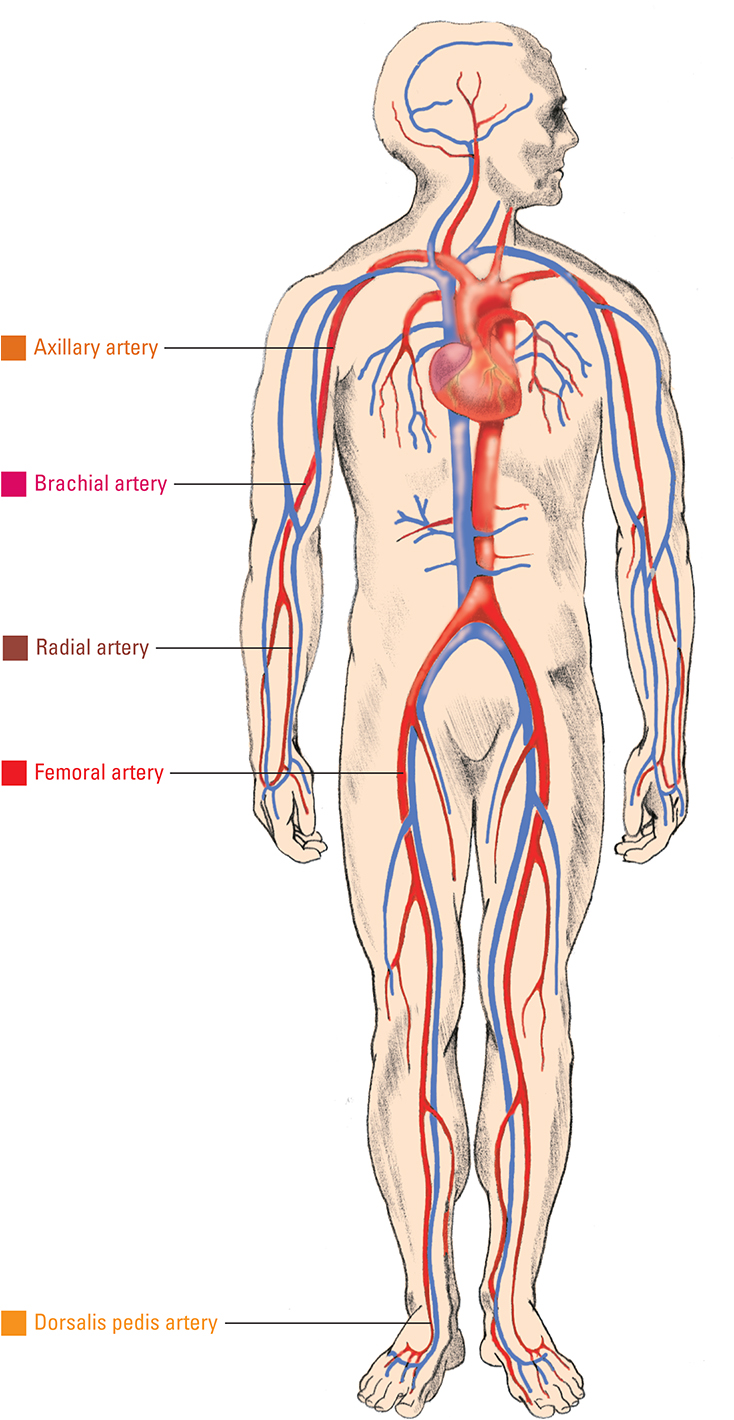

Choosing an arterial catheter site
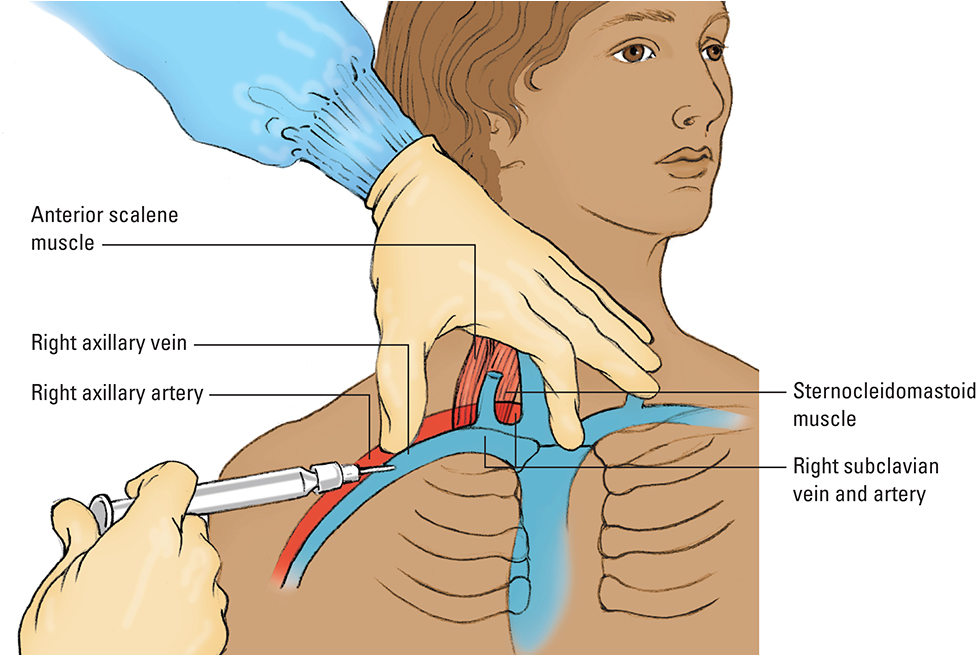
When your patient needs arterial pressure monitoring, an arterial catheter will probably be inserted in the radial artery. If these sites are unsuitable, the catheter may be inserted in the femoral, brachial, axillary, or dorsalis pedis artery. Regardless of the site chosen, it should have an artery large enough to accommodate the arterial catheter without impeding distal blood flow. It should also be free of infection or traumatic injury proximal to the insertion site. The insertion can also be facilitated using ultrasound-guided vascular access.
Advantages and disadvantages of each site are described in the following table.
Allen test
Before accessing the radial artery for peripheral arterial line insertion, the patient's ulnar and radial circulation must be checked for collateral circulation. Why? If the radial artery is blocked by a blood clot (a common complication of arterial lines), the ulnar artery alone must supply blood to the hand. A simple, reliable test of circulation can be done by performing the Allen test, which demonstrates how well both arteries supply blood to the hand.
Performing the Allen test
Follow these steps to perform the Allen test:
Rest the patient's arm on a flat surface, such as having the patient rest their arm at their side on the mattress or on the bedside stand. Support the patient's wrist with a rolled towel. Have them clench their fist. Then, using your index and middle fingers, palpate and then press both the radial and ulnar arteries. Hold this position for a few seconds.

Without removing your fingers from the patient's arteries, ask them to unclench their fist and hold their hand in a relaxed position. The palm will be blanched because pressure from your fingers has impaired the normal blood flow.

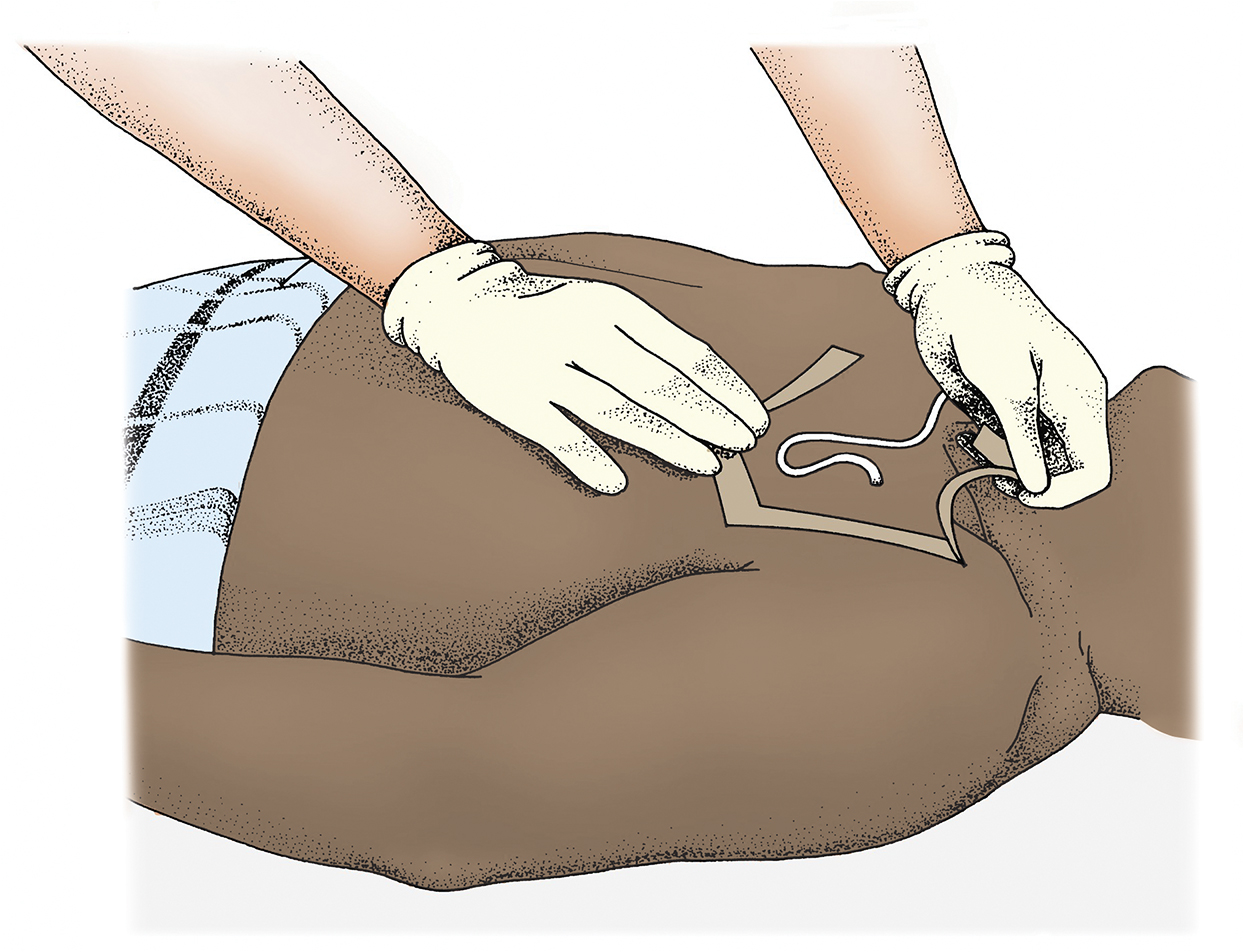
Release pressure on the patient's ulnar artery but keep pressure on the radial artery, as shown below. Observe the palm for a brisk return of color or "flushing," which should occur within 7 seconds (showing a patent ulnar artery and adequate blood flow to the hand). If color returns in 7 to 15 seconds, blood flow is impaired; if color returns after 15 seconds, consider the flow inadequate.

If blood flow is impaired or inadequate, the radial artery in this hand should not be used. At this point, proceed with the Allen test on the other hand. If neither hand colors or flushes, consider another site, such as the brachial artery, for catheter insertion.
Caring for arterial catheters
There are three steps to basic care for arterial catheters:
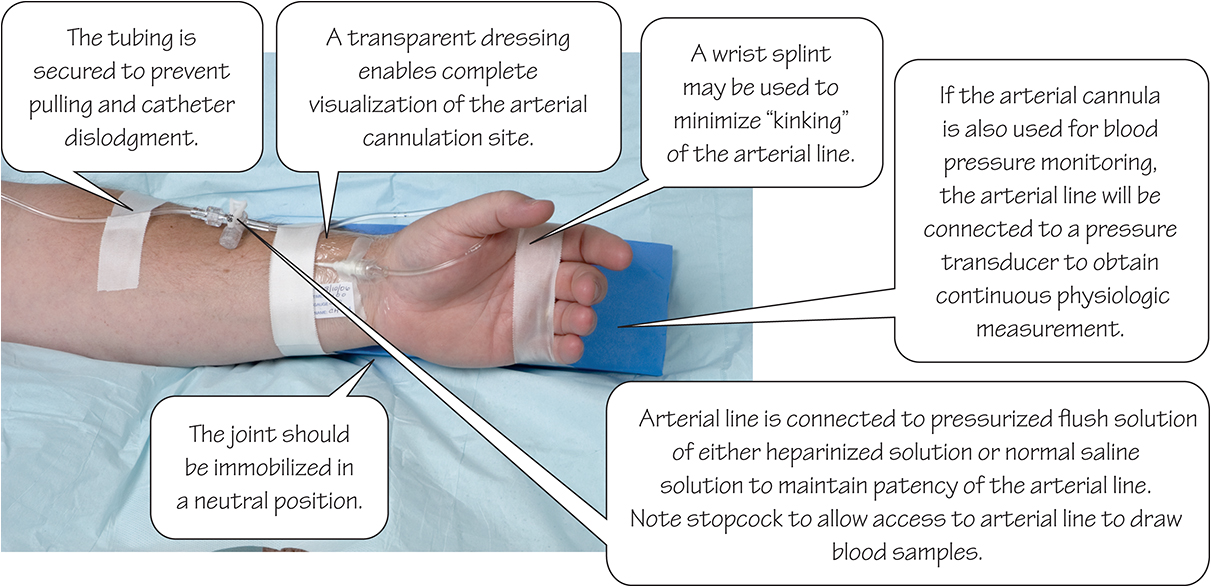
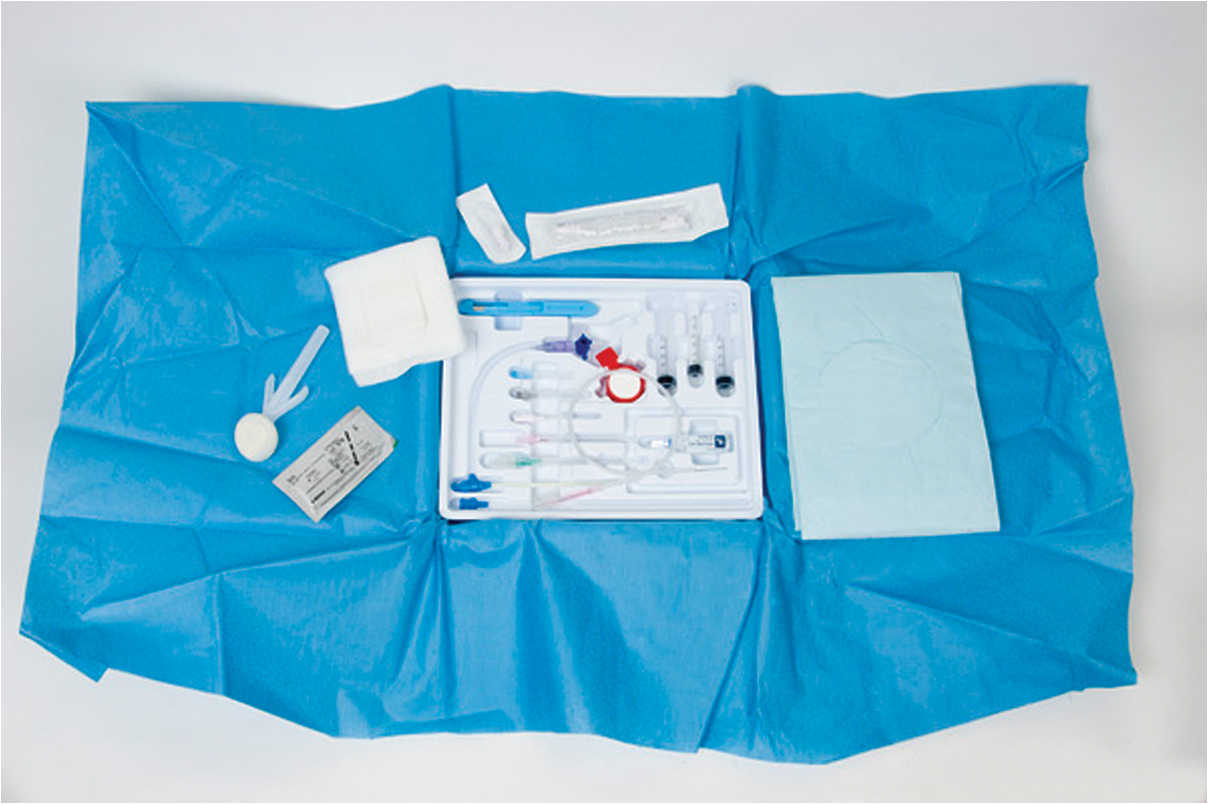
Dressing: After insertion of the arterial catheter, dress the insertion site and change it according to facility policy. Sterile dressing changes are recommended. Transparent dressings are typically used over the insertion site to enable complete visualization of the site. This breathable film allows oxygen in and moisture vapors out, while also providing barrier protection.
Immobilizing: The body part where the catheter is placed will then need to be immobilized. The joint or limb should be placed in a neutral position to prevent joint flexion or extension, which may result in kinking or dislodgment of the catheter. If the radial artery has been used, take care not to hyperextend the wrist, which could result in nerve or neuromuscular injury. Assess the limb with the arterial cannulation for any associated pressure points when immobilizing the extremity. Regularly assess the functioning of the arterial line to prevent kinking.
Assessing: The arterial catheter site must be assessed every hour. Include the following in your assessment:
Inspect the arterial catheter insertion site for redness, drainage, bruising, or blanching. (The benefit of using a transparent dressing becomes apparent at this step.) Palpate the area for firmness or swelling.
Assess circulation of the extremity in which the arterial catheter has been placed by evaluating skin color, temperature, capillary refill, distal pulses (if applicable), and motor and sensory function.
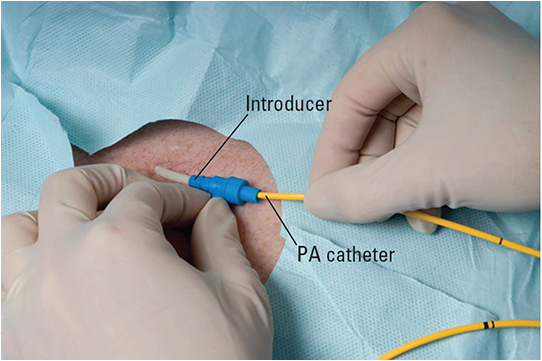
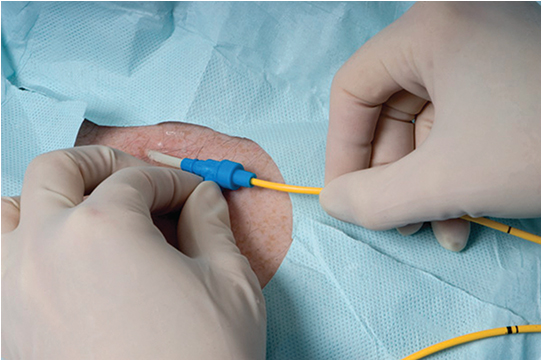
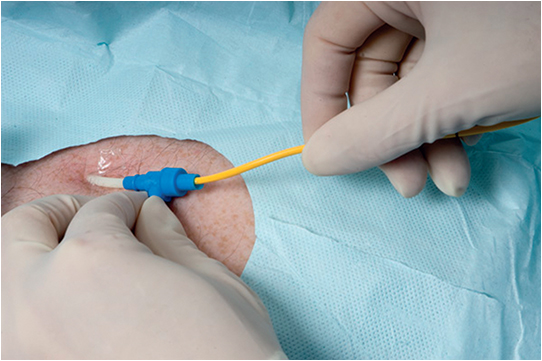
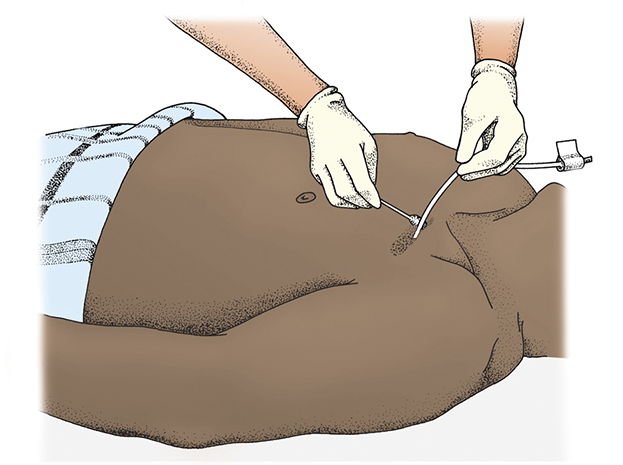
A closer look at an arterial line
This photograph shows an arterial line taped in place in the radial artery. (Flush is shown in Chapter 4.)