A child responds more rapidly and unpredictably to drugs than does an adult. Factors such as age, weight, body surface area, and drug form and route all play a part. Certain disorders can also affect a child's response to medication. For example, gastroenteritis increases gastric motility, which in turn impairs absorption of certain oral medications. Liver or kidney disorders can hinder the metabolism of some medications.
You may need to adjust usual drug administration techniques to account for the child's age, size, and developmental level. For example, the thin epithelium of a neonate or infant can absorb topical medications much faster than an older child. In addition, the injection site and needle size varies depending on the child's age and physical development.
For oral medications
Prescribed medication  disposable plastic syringe, plastic medicine dropper, or spoon
disposable plastic syringe, plastic medicine dropper, or spoon  medication cup
medication cup  water, syrup, or jelly (for tablets)
water, syrup, or jelly (for tablets)  optional: fruit juice.
optional: fruit juice.
For injectable medications
Prescribed medication  appropriately sized syringe and needle
appropriately sized syringe and needle  alcohol pads or povidone-iodine solution
alcohol pads or povidone-iodine solution  gloves
gloves  gauze pads
gauze pads  cold compresses
cold compresses  adhesive bandage.
adhesive bandage.
Check the doctor's order for the prescribed drug, dosage, and route. Compare the order with the drug label, checking the expiration date. Review for allergies.
When one isn't enough
Calculate the dosage to ensure proper milligram per kilogram amount, if necessary, and have another nurse verify it. Check your hospital's policy to learn which drugs must be calculated and checked by two nurses.
For giving an intramuscular injection, select the appropriate needle. (See Centers for Disease Control and Prevention recommendations for intramuscular injections.)
For subcutaneous injections, select a 23G to 25G 5/8'' needle and for intradermal medications, a 27G ½'' needle. To administer viscous medications, select a larger gauge needle.
Identify the child using two patient identifiers per facility policy validated with the medication administration record (MAR). If using the electronic MAR, scan the child's identification band and the medication to verify accuracy. If the child can talk and respond, ask him his name.
Explain the procedure and provide privacy.
Teach the patient/family about the medication, action, and side effects.
Perform hand hygiene.
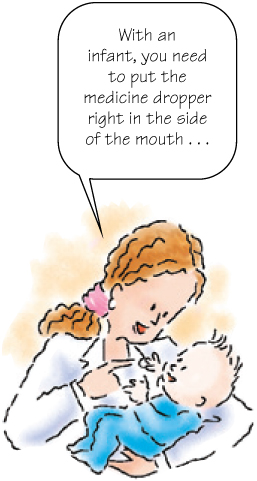
Giving oral medication to an infant
Use either a plastic syringe without a needle or a drug-specific medicine dropper to measure the dose. If the medication comes in tablet form, first crush the tablet (if appropriate) and mix it with water or syrup. Then draw the mixture into the syringe or dropper.
Pick up the infant, raising his head and shoulders or turning his head to one side, holding him close to your body.
Using your thumb, press down on the infant's chin and slide the syringe or medicine dropper into the infant's mouth alongside his tongue and let the medication slowly flow into the pocket between the cheek and gum.
Place the infant on his side or back or allow an active infant to assume a position that is comfortable for him.
Giving oral medication to a toddler
Use a disposable plastic syringe or plastic medicine dropper to measure liquid medication then transfer the fluid to a medication cup.
Elevate the toddler's head and shoulders.
The child may help hold the cup to enlist his cooperation. Otherwise, hold the cup to his lips or use a syringe or a spoon to administer the liquid. Make sure that the toddler ingests all of the medication.
If the medication is in tablet form, first crush the tablet, if appropriate, and mix it with water, syrup, or jelly. Use a spoon, syringe, or dropper to administer the medication. You may also offer a favorite drink to give after taking the medication.
Giving oral medication to an older child
If possible, let the child choose both the liquid medication mixer and a beverage to drink after taking the medication. If appropriate, allow him to choose where he will take the medication; for example, sitting in bed or sitting on a parent's lap.
A child between ages 4 and 6 may swallow solid medication, such as tablet or capsule form, by having him place it on the back of his tongue and swallow it immediately with water or juice. Look inside the child's mouth to confirm that he swallowed the pill.
If the child can't swallow the pill whole, crush it (if appropriate) and mix it with water, syrup, or jelly. Or, after checking with the child's doctor, order the medication in liquid form.

Giving an I.M. injection
Choose an injection site that's appropriate for the child's age and muscle mass. (See Centers for Disease Control and Prevention recommendations for intramuscular injections.)
Position the child appropriately for the site chosen and locate key landmarks, for example, the posterior superior iliac spine and the greater trochanter. Have someone help you restrain an infant; seek an older child's cooperation before enlisting assistance.
Perform hand hygiene and don gloves. Clean the injection site with an alcohol or povidone-iodine pad, wiping outward from the center with a spiral motion. If the child is older than 6 months, consider using topical anesthetic such as EMLA. Note that EMLA should be applied 1 hour before the intramuscular (I.M.) injection.
Grasp the tissue surrounding the site between your index finger and thumb and insert the needle quickly, using a darting motion at a 90-degree angle. If you're using the ventrogluteal site, insert the needle at a 45-degree angle toward the knee.
Aspirate the plunger to ensure that the needle is not in a blood vessel. If no blood appears, inject the medication slowly at 10 seconds/mL. Wait 10 seconds for the medication to absorb and withdraw the needle. To reduce injection site discomfort, there is no longer a need to aspirate after the needle is inserted when administering vaccines per the Centers for Disease Control and Prevention. Follow facility policy regarding aspirating after injecting the needle.
Withdraw the needle and gently massage the area with a gauze pad.
Provide comfort and praise.
Giving a subcutaneous injection
The middle third of the upper outer arm, the middle third of the upper outer thigh, or the abdomen may be used. You may apply a cold compress to the injection site to minimize pain.
Perform hand hygiene and don gloves. Prepare the injection site with alcohol or povidone-iodine solution.
Pinch the tissue surrounding the site between your index finger and thumb and hold the needle at a 45-degree angle. Quickly insert it into the tissue, release your grasp on the tissue, and slowly inject the medication. Remove the needle quickly and, unless contraindicated, gently massage the area.
Giving an intradermal injection
Put on gloves and pull the child's skin taut at the inner aspect of the forearm.
Insert the needle, bevel up, at a 10- to 15-degree angle just beneath the outer skin layer and slowly inject the medication, watching for a bleb to appear. Quickly remove the needle and draw a circle around the bleb, if required (such as in allergy testing). Avoid massaging the area.
Allow the child choices, if possible, such as choosing from the appropriate sites for an injection. You can also allow the child to play with a medication cup or syringe and to pretend to give medication to a doll.
It's the best policy
When giving medication to an older child, be honest. Reassure him that distaste or discomfort will be brief. Emphasize that he must remain still and that an assistant will help him to remain still if necessary. Keep your explanations brief and simple.
Certain medications are considered “high-alert medications” and should be double checked for accurate dosages with another nurse. Check the facility policy for high-alert medications. These include: digoxin, heparin, insulin, narcotics such as morphine, potassium and calcium, epidural medications, chemotherapy, sedation and anesthesia, and intravenous (I.V.) medications greater than 20% glucose.
Medal of honor
To divert the child's attention, have him start counting just before the injection and challenge him to try to reach 10 before you finish the injection. If the child cries, do not scold him or allow the parents to scold him. After the injection, have one of the parents hold a younger child and praise him for allowing you to give him the injection. You can also apply an adhesive bandage to the injection site as a form of reward or badge. Allow the child to select the Band-Aid he wants.
Return to the room in 15 to 20 minutes to check if there is any pain, burning, numbness, or tingling at the injection site.
Teach the parents about the proper dosage and administration of all prescribed medications. Use written materials to reinforce your teaching. (See Documenting drug administration.)
Outline