A.3. Describe IABP inflation and deflation timing.
Answer:
The balloon is connected to a control console that regulates inflation and deflation of the balloon at the tip of the IABP. The IABP balloon is inflated in diastole and deflated in systole. The triggers for balloon inflation are (1) the electrocardiogram (ECG) T wave; (2) the dicrotic notch on the arterial pressure waveform (as measured by a fluid-filled column), which is recorded from the tip of the IABP; and (3) in newer versions, a fiber-optic pressure manometer embedded in the tip of the IABP. Use of fiber-optic manometers and computerized waveform analysis allows better beat-to-beat cardiac support and minimizes artifacts. Balloon deflation is timed to occur prior to the ECG Q wave or the upstroke of the arterial pressure waveform (Figure 6.1). Improper IABP timing reduces effectiveness and can increase myocardial oxygen consumption. Early diastolic inflation of the IABP balloon (inflation is initiated during late systole) results in increased left ventricular (LV) afterload and increased myocardial oxygen consumption. Late diastolic inflation results in suboptimal coronary perfusion and diastolic augmentation. Examples of this include:
Figure 6.1.: One Complete Cardiac Cycle and the Corresponding Waveform of an Intra-Aortic Balloon Pump (IABP) during the Inflation and Deflation.
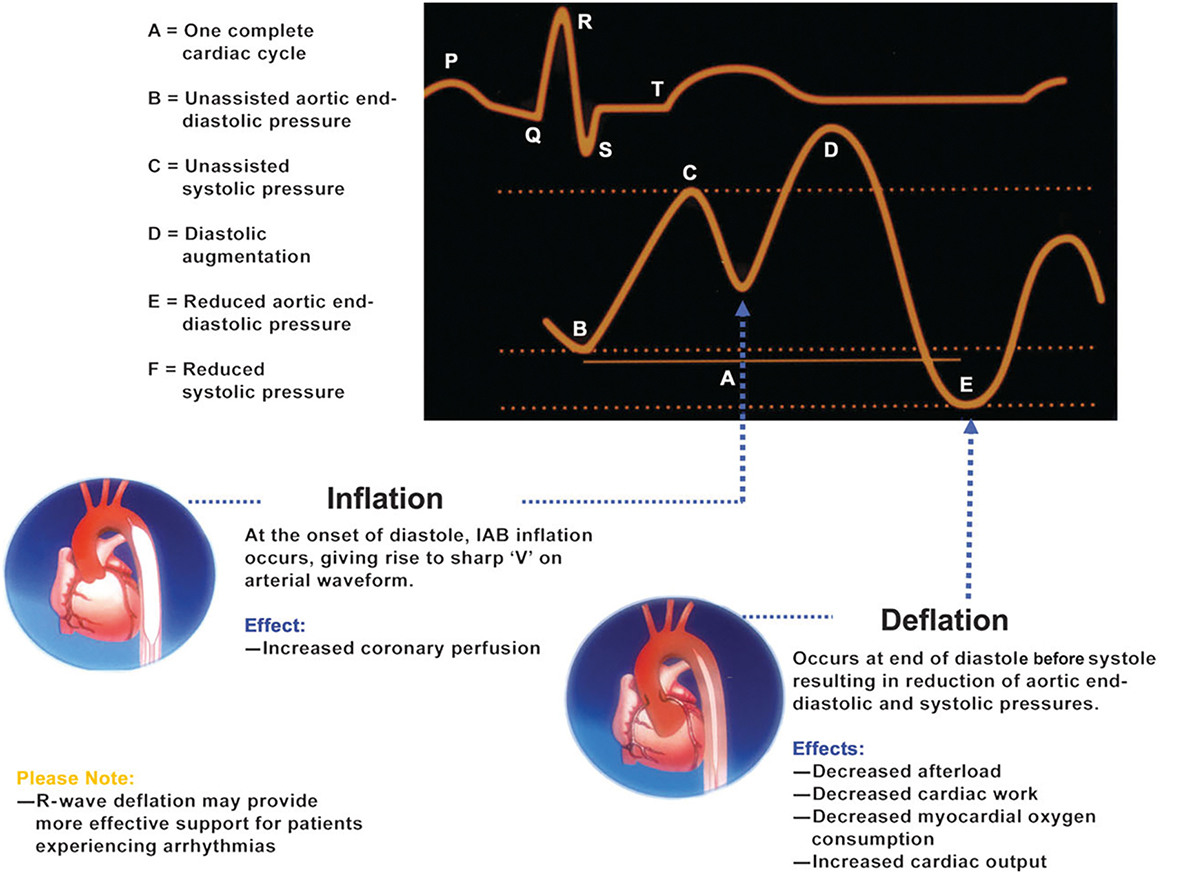
One complete cardiac cycle and the corresponding waveform of an intra-aortic balloon pump (IABP) during the inflation and deflation. (Reproduced with permission from Datascope®.)
Early inflation: inflation of the IABP before aortic valve closure (Figure 6.2A)
Late inflation: inflation of the IABP after closure of the aortic valve (Figure 6.2B)
Early deflation: premature deflation of the IABP during diastole (Figure 6.2C)
Late deflation: deflation of the IABP after the onset of systole (Figure 6.2D)
Figure 6.2.: A. Waveform Characteristics: Inflation of Intra-Aortic Balloon Pump (IABP) Before Dicrotic Notch; if Diastolic Augmentation Encroaches onto Systole, May Be Unable to Distinguish.
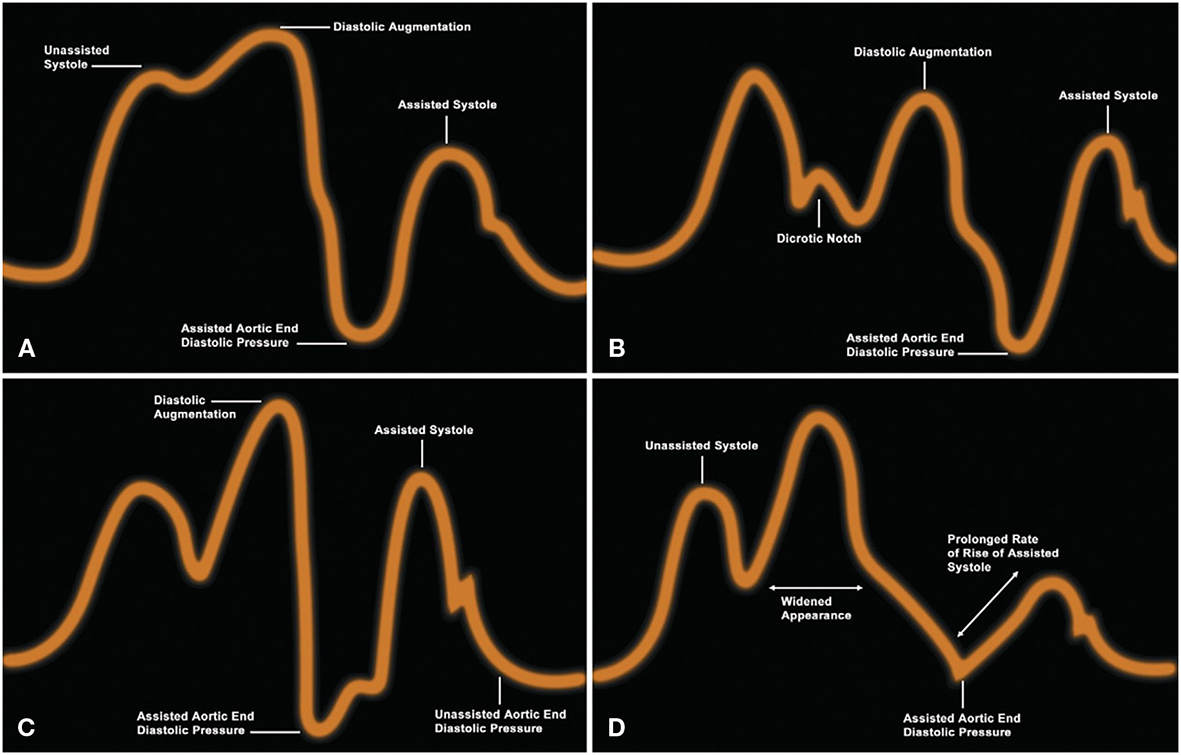
A. Waveform characteristics: inflation of intra-aortic balloon pump (IABP) before dicrotic notch; if diastolic augmentation encroaches onto systole, may be unable to distinguish. Physiologic effects: potential premature closure of the aortic valve; potential increase in left ventricular end-diastolic volume (LVEDV) and left ventricular end-diastolic pressure (LVEDP) or pulmonary catheter wedge pressure (PCWP); increased LV wall stress or afterload; aortic regurgitation; increased myocardial oxygen (MVO2) demand. B. Waveform characteristics: inflation of IABP after the dicrotic notch; absence of sharp "V." Physiologic effects: suboptimal coronary artery perfusion. C. Waveform characteristics: deflation of IABP is seen as a sharp decrease after diastolic augmentation; suboptimal diastolic augmentation; assisted aortic end-diastolic pressure can be equal to or less than the unassisted aortic end-diastolic pressure; assisted systolic pressure can increase. Physiologic effects: suboptimal coronary perfusion; potential for retrograde coronary and carotid blood flow; suboptimal afterload reduction; increased MVO2. D. Waveform characteristics: assisted aortic end-diastolic pressure can be equal to the unassisted aortic end-diastolic pressure; rate of increase of assisted systole is prolonged; diastolic augmentation can appear widened. Physiologic effects: afterload reduction is essentially absent; increased MVO2 because of the LV ejecting against a greater resistance and a prolonged isovolumetric contraction phase; IABP can impede LV ejection and increase afterload. (Reproduced with permission from Datascope®.)
References
- Boccellino A, Sacchi S, Pazzanese V, et al. Effects of intra-aortic balloon pump delayed deflation timing on carotid blood flow and cardiac mechanics: an ultrasound and haemodynamic study. J Heart Lung Transplant. 2023;42:451-455.
- Yarham G, Clements A, Morris C, et al. Fiber-optic intra-aortic balloon therapy and its role within cardiac surgery. Perfusion. 2013;28:97-102.


