Objectives ⬇
- Explore agency-based health information systems (ISs).
- Evaluate how administrators use core business systems in their practice.
- Assess the function and information output from selected ISs used in healthcare organizations.
Key Terms ⬆ ⬇
Introduction ⬆ ⬇
To compete in the ever-changing healthcare arena, organizations require quick and immediate access to a variety of types of information, data, and bodies of knowledge for daily clinical, operational, financial, and human resource activities. Information is continually shared between units and departments within healthcare organizations and is also required or requested from other healthcare organizations, regulatory and government agencies, educational and philanthropic institutions, and consumers. Organizations need interoperable systems that are accessible for data storage and retrieval.
But healthcare organizations are distinct from other organizations that use ISs. Fichman et al. (2011) identified six important elements of health care that may explain the lag in the development and implementation of ISs:
- The stakes are life and death.
- Healthcare information is highly personal.
- Health care is highly influenced by regulation and competition.
- Health care is professionally driven and hierarchical.
- Health care is multidisciplinary.
- Healthcare information system implementation is complex, with important implications for learning and adaptation. (pp. 420-423)
Healthcare organizations integrate a variety of clinical and administrative types of information systems (ISs). These systems collect, process, and distribute patient-centered data to aid in managing and providing care. Together, they create a comprehensive record of the patient's medical history and support organizational processes. Each of these systems is unique in the way it functions and provides information to clinicians and administrators. An understanding of how each of these types of systems works within healthcare organizations is fundamental in the study of informatics. This chapter will focus on the administrative organizational systems.
Principles of Interoperability ⬆ ⬇
It is important to realize that ISs of one type or another have been used in healthcare facilities for quite a while. Unfortunately, some of these early systems (sometimes referred to as legacy systems) created data silos; that is, the data and information central to that system remained in that system and could not easily be shared with other systems. A key component to coordinated, patient-centered care is the interoperability of healthcare ISs. Interoperability is defined as the ability of various systems and organizations to work together to exchange information. “Interoperability is made possible by the implementation of standards” (IEEE Standards University, 2016, para. 51). To provide continuity of care, data and information about our patients must be accessible and usable so that we are making informed decisions about their care. We also must monitor our patients, and often this requires gathering multiple biometric data from medical devices such as ventilators, blood pressure monitors, weight scales, and glucose monitors. By using IEEE standards, these devices can be interoperable. “A patient can access data from multiple devices at the same time and the provider can monitor all of the data to get a complete view of the patient's health” (IEEE Standards Association, 2023, para. 14). Metadata can be used to describe information about data and digital objects, using terms called tags. “Metadata tagging is the process of systematically assigning those tags to the digital assets in an archive or collection, typically using a rules-based system to ensure consistency” (MerlinOne, n.d.).
In 2015, the Office of the National Coordinator for Health Information Technology (ONC) released an interoperability road map to promote ease of access and use of electronic healthcare data. The final goal of the national road map emphasis on interoperability is driven by the need to “achieve nationwide interoperability to enable a learning health system, with the person at the center of a system that can continuously improve care, public health, and science through real-time data access” (ONC, 2015, p. vii). Since that time, the ONC sunsetted the road map ahead of schedule, but it did help “lay the groundwork and set the direction for policy development on information blocking, reducing provider burden, and nationwide, electronic health information exchange-to name a few” (Posnack, 2021b, para. 3). The Health Interoperability Outcomes 2030 will continue to drive this initiative. As an example, “because of interoperability, faxes are no longer used in clinical care before/by 2030. As another example, because of interoperability, before/by 2030 everyone that is part of a care team will have accurate, up-to-date clinical information prior to providing care” (Posnack, 2021a, para. 7). For more information on the synthesized statements that reflect the public's overall sentiments regarding 2030 outcomes, refer to the website at www.healthit.gov/topic/interoperability/health-interoperability-outcomes-2030. Glickman and Orlova (2022) recapped the standards development work that has been done over the past 16 years. This work has “led the International Organization of Standardization (ISO) Technical Committee 215, Health Informatics (ISO/TC 215) to the practical realization that a ‘bundle' of individual standards is required to create interoperable health information technology (health IT) standards that will ensure both adoption and sustainability” (para. 2).
As we develop more sophisticated electronic systems, we are realizing the huge potential benefits of exchanging secure and precise healthcare data. However, in the current landscape, several things need to happen to realize this goal. Chief among them is a worldwide commitment to interoperability. The Healthcare Information and Management Systems Society (HIMSS; n.d.) identified four types of health information technology (IT) interoperability-foundational, structural, semantic, and organizational-each with increasing complexity. Foundational interoperability defines the requirements necessary between systems to communicate data, and structural interoperability defines syntax and format to facilitate data exchange. Semantic interoperability is more complex and refers to consistency of clinical terminology and shared meanings. Finally, organizational interoperability refers to shared trust and consistency of policies and social and legal meanings to facilitate seamless workflows between organizations.
Suppose you have a joint replacement patient who is being discharged from the acute care facility to a rehabilitation center. You create a discharge summary for the patient in a PDF format and send it via a secure electronic exchange to the new facility. The staff at the rehabilitation center is able to read and understand the report, and a staff assistant can scan a copy of the discharge summary into the electronic record of the rehabilitation facility. This is an example of functional interoperability. If each facility uses Health Level 7 standards for data exchange and collects certain minimum data, then it might be possible for some data fields from one facility to populate automatically into an appropriate data field in the other facility. This is an example of structural interoperability. To achieve true sematic interoperability, systems must use the same standardized terminologies, or disparate terminologies must be mapped so that the two systems are able to “talk” to each other to exchange data seamlessly and to populate the data into the appropriate fields in the new system. True sematic interoperability enables machine-to-machine data exchange. The adoption and use will continue to need input from users to hone and evolve the standards so that they continue to meet each user's needs. We must strive to truly create the health interoperability ecosystem that “comprises individuals, systems and processes that want to share, exchange and access all forms of health information, including discrete, narrative and multimedia. Individuals, patients, providers, hospitals/health systems, researchers, payers, suppliers and systems are potential stakeholders within this ecosystem” (HIMSS, n.d., para. 29). It is imperative that every stakeholder be included in the “creation, exchange and use of health information and/or data. An efficient interoperability ecosystem provides an information infrastructure that uses technical standards, policies and protocols to enable seamless and secure capture, discovery, exchange and utilization of health information” (HIMSS, n.d., para. 29).
Types of Healthcare Organization Information Systems ⬆ ⬇
Case Management Information Systems
Case management information systems identify resources, patterns, and variances in care to prevent costly complications related to chronic conditions and to enhance the overall outcomes for patients with chronic illness. These systems scan past episodes of treatment and search for trends among the records. Once a trend is identified, case management systems provide decision support that promotes preventive care. Care plans are a common tool found in case management systems. A care plan is an evidence-based set of care guidelines that outline the course of treatment and the recommended interventions that should be implemented to achieve optimal results. By using a standardized plan of care, these ISs present clinicians with treatment protocols to maximize patient outcomes and support best practices. IT in health care is positioned to support the development of interdisciplinary care plans. In the health informatics pathway, Standard 5 deals with documentation, for which AHIMA (2020) stated the importance of actively participating in the “development of query policies that support documentation integrity, and meet regulatory, legal, and ethical standards for coding and reporting” (para. 22). We are all responsible for accurate documentation and being aware of the varied uses of healthcare information. As we interact with the interdisciplinary healthcare team verbally and in writing when we document information about our patients, it is imperative that we adhere to the legal and regulatory standards that promote truthful and ethical reporting methods, resulting in correct and trustworthy data and information.
Case management information systems are especially beneficial for patient populations with a high cost of care and complex health needs, such as the elderly or patients with chronic disease conditions. Avoiding complications requires identifying the right resources for care and implementing preventive treatments across all medical visits. The more information that can be shared among all types of providers, the more that care planning and decision-making can be coordinated, consistent, and safe. Ultimately, this coordinated care decreases the costs of care for patients with chronic illnesses and supports a better quality of life. Such systems increase the value of individual care while controlling the costs and risks associated with long-term health care. Initially, case managers were employed by hospitals, and they primarily focused on utilization review and discharge planning. Now case managers are practicing in other arenas, including home health agencies and insurance companies (Davis, 2022). Case management systems are increasingly being integrated with electronic health records (EHRs). Information collected by these systems is processed in a way that helps to reduce risks, ensure quality, and decrease costs.
In an effort to promote patient-centered care for the management of chronic diseases, Fico et al. (2016) reported on the development of an information and communication technology platform to support personalized healthcare pathways to manage diabetes. The system they developed and tested allowed for automatic data collection via personal monitoring devices worn by the patient. Using standardized treatment plans and system analysis of patient data, “the system delivers automated feedback consisting of alerts, reminders, and motivational messages in real time and periodically (over three and seven days' period)” (Fico et al., 2016, p. 30). Phamily (n.d.) integrates its chronic care management service into your EHR and provides a “unique texting-based approach to patient engagement” (para. 1). MCG Health offers assessments for people experiencing chronic conditions and high-intensity and low-intensity guidelines for disease management along with patient engagement tools (Miller, 2023). These examples show the types of case management tools being developed for chronic disease management within and outside of the healthcare system.
Communication systems promote interaction among healthcare providers and between providers and patients and are designed to be Health Insurance Portability and Accountability Act (HIPAA) compliant. Such systems have historically been kept separate from other types of health ISs and from one another. Healthcare professionals overwhelmingly recognize the value of these systems, however, so they are now more commonly integrated into the design of other types of systems as a newly developing standard within the industry. There is no one size fits all for communication systems. According to Mock (2021), “the log-out mechanisms in provider-to-provider systems make them impractical for emergency alerts, while the capabilities of provider-to-patient systems (or vice versa) do not support mass notification” (para. 15). Examples of communication systems include call light systems, wireless telephones, pagers, email, and instant messaging, which have traditionally been forms of communication targeted at clinicians. Other communication systems target patients and their families. Some patients are now able to access their electronic chart from home via an internet connection. They can update their own medical record to inform their physician of changes to their health or personal practices that affect their physical condition. Inpatients in hospital settings also receive communication directly to their room. Patients and their families may, for example, review individualized messages with scheduled tests and procedures for the day and confirm menu choices for their meals. These types of systems may also communicate educational messages, such as smoking cessation advice.
With the introduction of more of these technologies into practice, the value of having communication tools integrated with other types of systems is being widely recognized. Integrating communication systems with clinical applications provides a real-time approach that facilitates interactions among the entire healthcare team and patients and their families to enhance care. These systems improve the flow of communication within an organization and promote an exchange of information to better care for patients. The next generation of communication systems will be integrated with other types of healthcare systems and guaranteed to work together smoothly. The following Research Briefs from 2010, 2014, and 2020 discuss the economic and quality healthcare effect of communication inefficiencies in U.S. hospitals. As hospitals and physician practices strive to become more patient centered, communication technologies will be an integral part of this goal. Many of us have experienced the anxiety of waiting for news about a loved one during a surgical procedure. Newer communication techniques, such as surgical tracking boards that communicate about the process, help to ease these anxieties. Gordon and colleagues (2015) reported high patient and family satisfaction with a HIPAA-compliant surgical instant messaging system to communicate real-time surgical progress with patient-designated recipients. Post-COVID-19 pandemic conditions continue to affect communication styles and challenge healthcare professionals to demand unified communications (UC) in health care. Carter (2022) stated that the UC “market will grow at a rate of 18.3% in the healthcare space up to the year of 2026, enabling the sector to provide a better quality of patient care” (para. 2).
What are some other ways that new communication technologies could be harnessed into a UC interface and leveraged to increase patient and family satisfaction with health care in your practice?
| Research Briefs |
|---|
| 2010 |
|---|
| Researchers attempted to quantify the costs of poor communication, termed communication inefficiencies, in hospitals. This qualitative study was conducted in seven acute care hospitals of varying sizes via structured interviews with key informants at each facility. The interview questions focused on four broad categories: (1) communication bottlenecks, (2) negative outcomes as a result of those bottlenecks, (3) subjective perceptions of the potential effectiveness of communication improvements on the negative outcomes, and (4) ideas for specific communication improvements. The researchers independently coded the interview data and then compared results to extract themes.
All the interviewees indicated that communication was an issue. Inefficiencies revolved around time spent tracking people down to communicate with them, with various estimates provided: 3 hours per nursing shift wasted tracking people down, 20% of productive time wasted on communication bottlenecks, and a reported average of five to six telephone calls to locate a physician. Several respondents pointed to costly medical errors that were the direct result of communication issues. Communication lapses also resulted in inefficient use of clinician resources and increased length of stay for patients.
The researchers developed a conceptual model of communication quality with four primary dimensions: (1) efficiency of resource use, (2) effectiveness of resource use, (3) quality of work life, and (4) service quality. They concluded that the total cost of communication inefficiencies in U.S. hospitals is more than $12 billion annually and estimated that a 500-bed hospital could lose as much as $4 million annually because of such problems. They urge the adoption of information technologies to redesign workflow processes and promote better communication. It would be interesting to see this study repeated today to ascertain whether these inefficiencies still exist despite the introduction of newer technologies.
The full article appears in: Agarwal, R., Sands, D., Schneider, J., & Smaltz, D. (2010). Quantifying the economic impact of communication inefficiencies in U.S. hospitals. Journal of Healthcare Management, 55(4), 265-281.
|
| 2014 |
|---|
| The Ponemon Institute (2014) surveyed more than 400 U.S. healthcare providers about the conventional communication process during three clinical workflows: coordinating emergency response, admitting patients, and transferring patients. There was overwhelming agreement among the participants that significant time was wasted during each workflow basically because of ineffective communications having an “estimated annual economic impact of about $1.75 million per U.S. hospital and more than $11 billion industry-wide” (Ponemon Institute, 2014, para. 4). |
| 2020 |
|---|
| Dinsdale et al. (2020) analyzed data from 3,293 referral letters and 2,468 response letters from 68 general practices and 17 hospitals in addition to 6,800 patients' files over a 2-year period.
The authors identified several “areas for improvement at different points in the patient journey in the context of increasing complexity in medicine due to chronic disease and multi-morbidity” (Dinsdale et al., 2020, p. 67). It was interesting to note that there were communication gaps caused by the length of time it took to deliver letters from the hospital to general practitioners. The authors stressed that “it is possible to adopt appropriate evidence-based strategies to improve the quality and timeliness of referral and response letters. Future research should be aimed at developing robust strategies to addressing communication gaps reported in this study” (Dinsdale et al., 2020, p. 67).
Dinsdale, E., Hannigan, A., O'Connor, R., O'Doherty, J., Glynn, L., Casey, M., Hayes, P., Kelly, D., Cullen, W., & O'Regan, A. (2020). Communication between primary and secondary care: Deficits and danger. Family Practice, 37(1), 63-68. https://doi.org/10.1093/fampra/cmz037
|
Core Business Systems ⬆ ⬇
Core business systems enhance administrative tasks within healthcare organizations. Unlike clinical information systems (CISs), whose aim is to provide support for direct patient care, these systems support the administrative management of health care within an organization. Core business systems provide the framework for reimbursement, support of best practices, quality control, and resource allocation. There are four common core business systems: (1) admission, discharge, and transfer (ADT) systems; (2) financial systems; (3) acuity systems; and (4) scheduling systems.
Admission, discharge, and transfer (ADT) systems provide the backbone structure for the other types of clinical and business systems and, when automated, provide opportunities for health information exchange leading to care coordination (Michigan Health Information Network, 2019). These systems were among the first to be automated in health care. Admitting, billing, and bed management departments most commonly use ADT systems within the hospital setting. These systems hold key information on which all other systems rely. For example, ADT systems maintain the patient's name; medical record number; visit or account number; and demographic information, such as age, gender, home address, and contact information. Such systems are considered the central source for collecting this type of patient information and communicating it to other types of healthcare ISs. Initially, these systems were primarily in-house management systems, but with the national health IT expansion, ADT systems may communicate important information about patient transitions (i.e., admissions, discharges, and/or emergency room visits) to the primary care physician, insurance company, community case manager, or skilled nursing and rehabilitation facilities. The ADT alert system was designed to improve communication across care providers, improve chronic care patient management, and reduce unnecessary hospital utilization (Michigan Health Information Network, n.d.; ONC, 2013). The ADT notifications help to determine overutilization and provide the information necessary for healthcare providers to intervene by identifying those patients who repeatedly access the healthcare system. Once identified, the provider can assist these super user, high utilizer, or super-high utilizer patients by affording both clinical and nonclinical options or interventions. The goal is to decrease the amount of overutilization by avoiding or preventing visits to the emergency room as well as readmissions to the hospital (Gilbert et al., 2018; Maruster et al., 2021; Tsai et al., 2018).
HealthShare Exchange (n.d.) in Philadelphia collects ADT data from 39 hospitals and makes it possible to track patients receiving services from multiple providers, thus promoting coordinated care and care efficiencies. Even in long-term care, “[c]loud-based ADT message systems can now be synched with handheld devices, giving caregivers access to a resident's medical data on the go. There has also been considerable improvement in data entry accuracy as well as improved data organization” (Wong, 2022, para. 5).
Financial systems manage the expenses and revenue for providing health care. The finance, auditing, and accounting departments within an organization most commonly use financial systems. These systems determine the direction for maintenance and growth for a given facility. They often interface to share information with materials management, staffing, and billing systems to balance the financial effect of these resources within an organization. Financial systems report fiscal outcomes, which can then be tracked and related to the organizational goals of an institution. These systems are key components in the decision-making process as healthcare institutions prepare their fiscal budgets. They often play a pivotal role in determining the strategic direction for an organization.
Acuity systems monitor the range of patient types within a healthcare organization using specific indicators. They track these indicators based on the current patient population within a facility. By monitoring the patient's acuity, these systems provide feedback about how intensive the care requirement is for an individual patient or for a group of patients. Identifying and classifying a patient's acuity can promote better organizational management of the expenses and resources necessary to provide quality care. Information about a patient's acuity also provides important insights into staffing for safe care delivery. Acuity systems help predict the ability and capacity of an organization to care for its current population. They also forecast future trends to allow an organization to successfully strategize on how to meet upcoming market demands. Trepanier et al. (2017) reported on the implementation of a value-based nurse staffing model using a data-driven, interoperable acuity-based staffing (ABS) system. “Sophisticated ABS technology offers many new and exciting options that are significantly more accurate and less burdensome than the traditional staffing process. Such systems not only improve value to patients by supporting the achievement of consistently better outcomes across the healthcare system, but they also provide reliable data to inform a variety of day-to-day and long-term planning and management tasks” (p. 188). Handzel (2021) described the nurse and non-nurse support staffing changes that were done in response to the COVID-19 pandemic. To increase responsiveness, several changes were made, such as creating a 1:4 ratio of nurses to patients and increasing the use of non-nurse support personnel. Also, “[a]lternative med/surg suites were prepared in the radiology care unit, CCL [cardiac catheterization lab], and two GI [gastrointestinal] procedural centers” (Handzel, 2021, para. 9).
Scheduling systems coordinate staff, services, equipment, and allocation of patient beds. They are frequently integrated with the other types of core business systems. By closely monitoring staff and physical resources, these systems provide data to the financial systems. For example, resource-scheduling systems may provide information about operating room use or availability of intensive care unit beds and regular nursing unit beds. These systems also provide great assistance to financial systems when they are used to track medical equipment within a facility. Procedures and care are planned when the tools and resources are available. Scheduling systems help to track resources within a facility while managing the frequency and distribution of those resources.
Increasingly, hospital systems are moving to enterprise resource planning (ERP) software that integrates many of the core business functions into one package, thus providing seamless access to data that can be used for planning, mandatory reporting, and overall strategic management purposes. “Implementing an ERP system can provide significant benefits for healthcare providers, not only in the promotion of proficient performance and functionality, but also in positioning organizations to respond to a quickly evolving industry” (DeLeon, n.d., para. 12).
Order Entry Systems ⬆ ⬇
Order entry systems are one of the most important systems in use today. They automate the way that orders have traditionally been initiated for patients; that is, clinicians place orders using these systems instead of creating traditional handwritten transcriptions onto paper. Order entry systems provide major safeguards by ensuring that physician orders are legible and complete, thereby providing a level of patient safety that was historically missing with paper-based orders. Computerized physician (or provider) order entry (CPOE) systems provide decision support and automated alert functionality that was unavailable with paper-based orders.
In the seminal report by the Institute of Medicine (2000), To Err Is Human: Building a Safer Health System, it was estimated that medical errors cost the United States approximately $37.6 billion each year; nearly $17 billion of those costs are associated with preventable errors. Consequently, the federal Agency for Healthcare Research and Quality Patient Safety Network (2019) continued to recommend eliminating reliance on handwriting for ordering medications and advocated instead for CPOE paired with clinical decision support. Because of the global concern for patient safety as a result of incorrect and misinterpreted orders, healthcare organizations are incorporating order entry systems into their operations as a standard tool for practice. Such systems allow for clear and legible orders, thereby promoting patient safety and streamlining care.
Patient Care Support Systems ⬆ ⬇
Most specialty disciplines within health care have an associated patient care information system. These patient-centered systems focus on collecting data and disseminating information related to direct care. Several of these systems have become mainstream types of systems used in health care. The four systems most commonly encountered in health care are (1) clinical documentation systems, (2) pharmacy information systems, (3) laboratory information systems, and (4) radiology information systems.
Clinical documentation systems, also known as clinical information systems (CISs), are the most commonly used type of patient care support system within healthcare organizations. CISs are designed to collect patient data in real time. They enhance care by putting data at the clinician's fingertips and enabling decision-making where it needs to occur, which is at the bedside. For that reason, these systems often are easily accessible at the point of care for caregivers interacting with the patient. CISs are patient centered, meaning they contain the observations, interventions, and outcomes noted by the care team. Team members enter information, such as the plan of care, hemodynamic data, laboratory results, clinical notes, allergies, and medications. All members of the treatment team use CISs; for example, pharmacists, allied health workers, nurses, physicians, support staff, and many others access patients' clinical records using these systems. Accuracy and thoroughness of clinical documentation are increasingly emphasized because the quality of documentation is now tied to reimbursement. Because of this, larger health systems began employing clinical documentation improvement (CDI) specialists, who review electronic records for gaps and inaccuracies in charting (Miliard, 2017). These specialists generally have both clinical and coding backgrounds so that they can review the medical records or documentation for missing data and information in relation to the disease process, diagnostics, and coding (AAPC, 2023).
Frequently, these clinical documentation systems are also referred to as the electronic patient record, or electronic health record (EHR).
Pharmacy information systems also have become mainstream patient care support systems. They typically allow pharmacists to order, manage, and dispense medications for a facility. They also commonly incorporate information regarding allergies and height and weight to ensure effective medication management. Pharmacy information systems streamline the order entry, dispensing, verification, and authorization process for medication administration. They often interface with clinical documentation and order entry systems so that clinicians can order and document the administration of medications and prescriptions to patients while having the benefits of decision-support alerting and interaction checking. Technologies emerging in pharmacy information systems include automated dispensing cabinets, CPOE, smart pumps, bar-coded medication administration (BCMA) systems, bar-coded unit dose packaging systems, and temperature monitoring systems. Halvorsen (2018) was correct in suggesting that the use of robotics was a trend worth watching. MarketWatch (2023) stated that the “global robotic prescription dispensing systems market is anticipated to rise at a considerable rate during the forecast period, between 2022 and 2030” (para. 1).
Laboratory information systems were perhaps some of the first CISs ever used in health care. Because of their long history of use within medicine, laboratory systems have been models for the design and implementation of other types of patient care support systems. Laboratory information systems report on blood, body fluid, and tissue samples along with biological specimens collected at the bedside and received in a central laboratory. They provide clinicians with reference ranges for tests indicating high, low, or normal values to make care decisions. Often, the laboratory system provides result information in the EHR and directs clinicians toward the next course of action within a treatment regimen. As older legacy systems are phased out, new laboratory information systems are designed to be fully interoperable with other health ISs, thus reducing turnaround times for specimen collection, transport, and analysis and providing opportunities for data analysis beyond basic results reporting (Muin, 2017). Interoperability of the laboratory information system is critical in the “move to interoperable healthcare systems because of the tremendous amount of data it manages and the value of that data in making patient care decisions” (Futrell, 2021, para. 1). The final type of patient care support system commonly found within health care is the radiology information system (RIS) used in radiology departments. These systems schedule, provide results, and store information related to diagnostic radiology procedures. One feature found in most radiology systems is a picture archiving and communication system (PACS). The PACS may be a stand-alone system, which is kept separate from the main radiology system, or it can be integrated with the RIS and CIS. These systems collect, store, and distribute medical images, such as computed tomography scans, magnetic resonance images, and X-rays. PACS replaces traditional hard copy films with digital media that are easy to store, retrieve, and present to clinicians. The benefit of RIS and PACS is their ability to assist in diagnosing and storing vital patient care support data. Imaging studies can be available in minutes as opposed to 2 to 6 hours for images in a film-based system. The digital workstations provide enhanced imaging capabilities and on-screen measurement tools to improve diagnostic accuracy. Finally, the archive system stores images in a database that is readily accessible so that images can be easily retrieved and compared to subsequent testing or shared instantly with consultants. Advances in RIS/PACS systems include the use of machine learning techniques to analyze data and create decision-support mechanisms. Brink et al. (2017) suggested that “[t]he use of machine learning promises better decision support for medical imaging, improved quantitative imaging, improved computer-assisted diagnoses, improved computer-assisted radiology for structured report generation, precision in diagnosis, and real-time correlation with other medical data” (p. 3649). However, Rockall (2019) provided a caution about the use of artificial intelligence (AI) and machine learning in radiology: “The key is to ensure that AI is used to address important unmet clinical needs, whether in relation to triage and diagnostic tools, improved workflow or sustainability of healthcare. Applications of AI must primarily serve patient needs, not just what's interesting or feasible” (p. 1). AI will greatly enhance and augment the field of radiology but not replace radiologists as once thought.
The mobility of patients both geographically and within a single healthcare delivery system challenges ISs because data must be captured wherever and whenever the patient receives care. In the past, managed care information systems were implemented to address these issues. Consequently, data can be obtained at any and all of the areas where a patient interacts with the healthcare system. Patient-tracking mechanisms continue to be honed, but the financial impact of health care also has changed these systems to some extent. The ISs currently in use enable nurses and physicians to make clinical decisions while being mindful of their financial ramifications. In the future, vast improvements in ISs and systems that support health information exchange are likely to continue to emerge.
One such trend is the incentive to develop accountable care organizations (ACOs), which are encouraged by the Patient Protection and Affordable Care Act of 2010. According to the Centers for Medicare and Medicaid Services (2020), “Accountable Care Organizations (ACOs) are groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high quality care to their Medicare patients. The goal of coordinated care is to ensure that patients, especially the chronically ill, get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors” (para. 1-2). Members of an ACO share data and information to better coordinate care and share in any healthcare cost savings generated when the coordination of care reduces unnecessary and duplicated costs.
Aggregating Patient and Organizational Data ⬆ ⬇
Many healthcare organizations now aggregate data in a data warehouse for the purpose of mining the data to discover new relationships and build organizational knowledge. Proper access to the data and big data analyses are critical to improving patient outcomes and healthcare processes. Data storage strategies can not only impact how data is made available to users and applications but also the success of any data analysis.
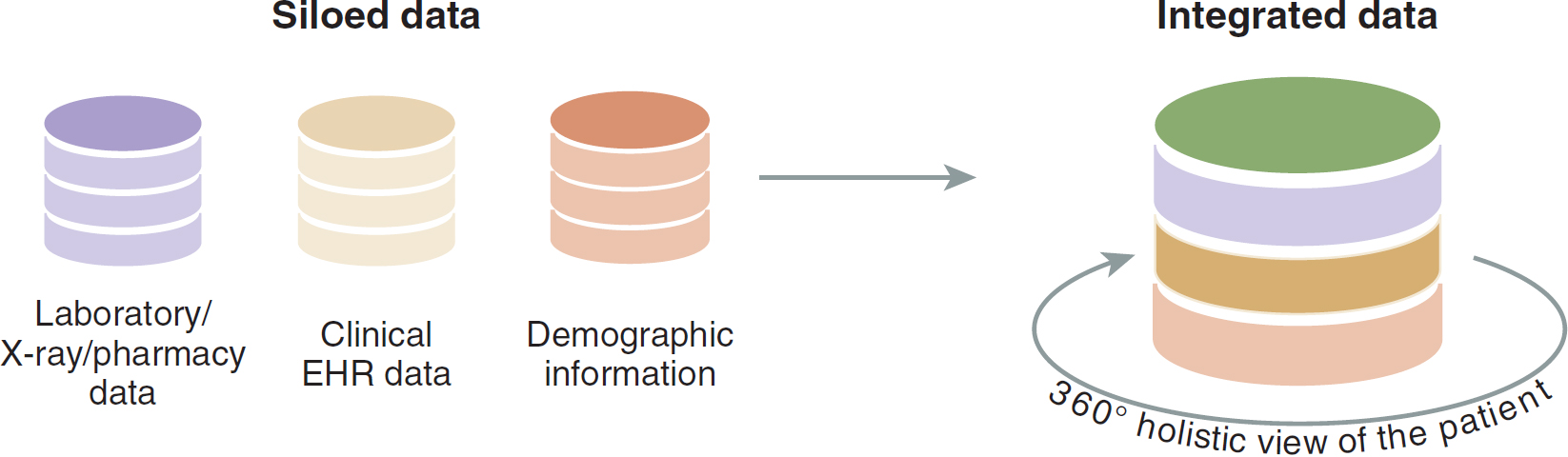
In addition to the access and storage challenges, “the information collected and generated by hospitals is managed and stored following the set standards” (Kholodenko, 2022, para. 56): HIPAA, electronic protected health information (EPHI), and Health Information Technology for Economic and Clinical Health (HITECH) Act. When disparate ISs within an organization are unable to interface with any other ISs (either within or outside of the organization), the result is poor communication, billing errors, and issues with continuity of care. By developing a single comprehensive database, healthcare systems are able to facilitate interprofessional communications yet maintain compliance with privacy regulations. Figure 10-1 depicts moving from siloed to integrated data.
Figure 10-1 Moving From Data Silos to Integrated Data
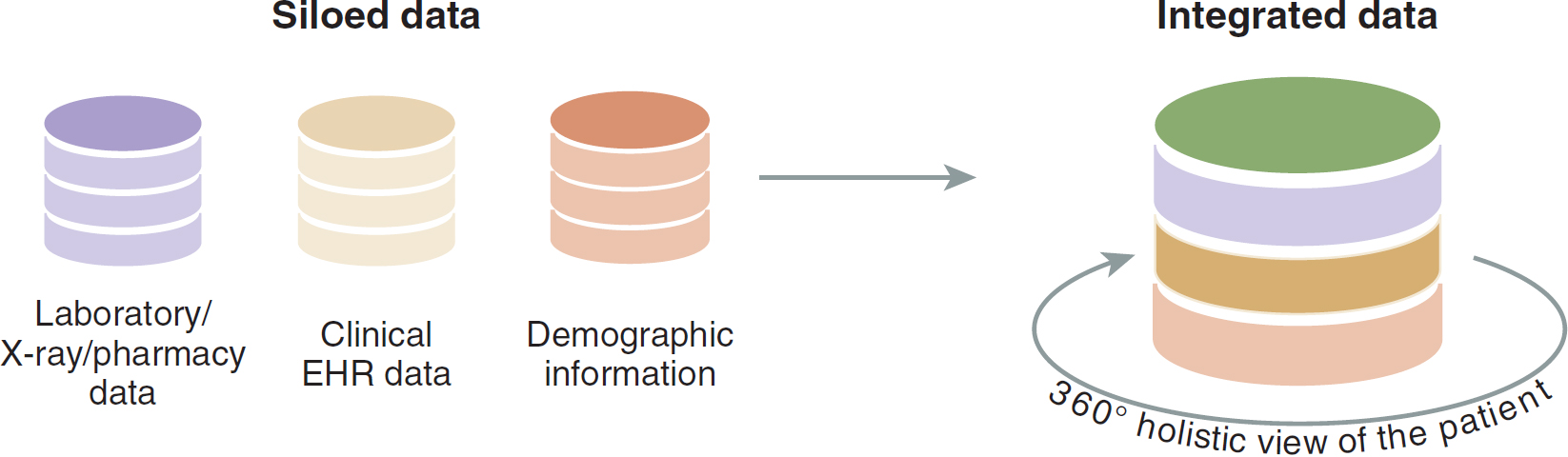
An illustration depicts the transition from siloed to integrated data.
The siloed data includes laboratory, X-ray, pharmacy data; clinical E H R data; and demographic information. When combined, these data sources create integrated data, providing a comprehensive 360-degree holistic view of the patient.
Data from: SmartData Collective. (2015, October 5). Two critical obstacles facing retailers for data driven marketing. www.smartdatacollective.com/two-critical-obstacles-facing-retailers-data-driven-marketing
Based on the size of the organization, data triage and tiering might be necessary. These decision-making processes related to data storage are based on predictions regarding how quickly data might need to be accessed. For example, consider the case of Intermountain, a chain of 22 hospitals in Salt Lake City. With 4.7 petabytes of data under its management, cloud storage becomes cost prohibitive. The network estimates the size of the hospital chain's data will grow by 25% to 30% each year until it reaches 15 petabytes 5 years from now (DeGaspari, 2013, para. 1).
With such massive data needs, it was imperative that Intermountain find ways to cut costs and streamline efficiency. One way was through data tiering, which is the creation of data storage tiers that can be accessed when necessary at the appropriate speeds. Tiering can be done manually through triaging but is typically accomplished through auto-tiering, which automatically stores data according to availability needs. Therefore, auto-tiering determines the media storage necessary to meet the data needs and can be a cost saver by storing data on lower-cost media when appropriate.
The most basic element of a database system is the data. Data refer to raw facts that can comprise unorganized text, graphics, sound, or video. Information is data that have been processed, meaning the data have been organized in a way that people find meaningful and useful. Even useful information can be lost if one is mired in unorganized information. Computers can come to the rescue by helping to create order out of chaos. Computer science and information science are designed to help cut down the amount of information to a more manageable size and organize it so that users can cope with it more efficiently through the use of databases and database program technology. Learning about basic databases and database management programs is paramount so that users can apply data and information management principles in health care.
A database is a structured or organized collection of data that is typically the main component of an IS. Databases and database management software allow the user to input, sort, arrange, structure, organize, and store data and turn those data into useful information. An individual can set up a personal database to organize recipes, music, names and addresses, notes, bills, and other data. In health care, databases and ISs make key information available to healthcare providers and ancillary personnel to promote the provision of quality patient care. Box 10-1 provides a detailed description of a database.
| Box 10-1 Overview of Database Construction |
|---|
| Databases consist of fields, or columns, and records, or rows. Within each record, one of the fields is identified as the primary key, or key field. This primary key contains a code, name, number, or other information that acts as a unique identifier for that record. In the healthcare system, for example, a patient is assigned a patient number, or ID, that is unique for that patient. As you compile related records, you create data files, or tables. A data file is a collection of related records. Therefore, databases consist of one or more related data files or tables.
An entity represents a table, and each field within the table becomes an attribute of that entity. The database developer must critically think about the attributes for each entity. For example, the entity disease might have the attributes of chronic disease, acute disease, or communicable disease. The name of the entity, disease, implies that the entity is about diseases. The fields, or attributes, are chronic, acute, or communicable.
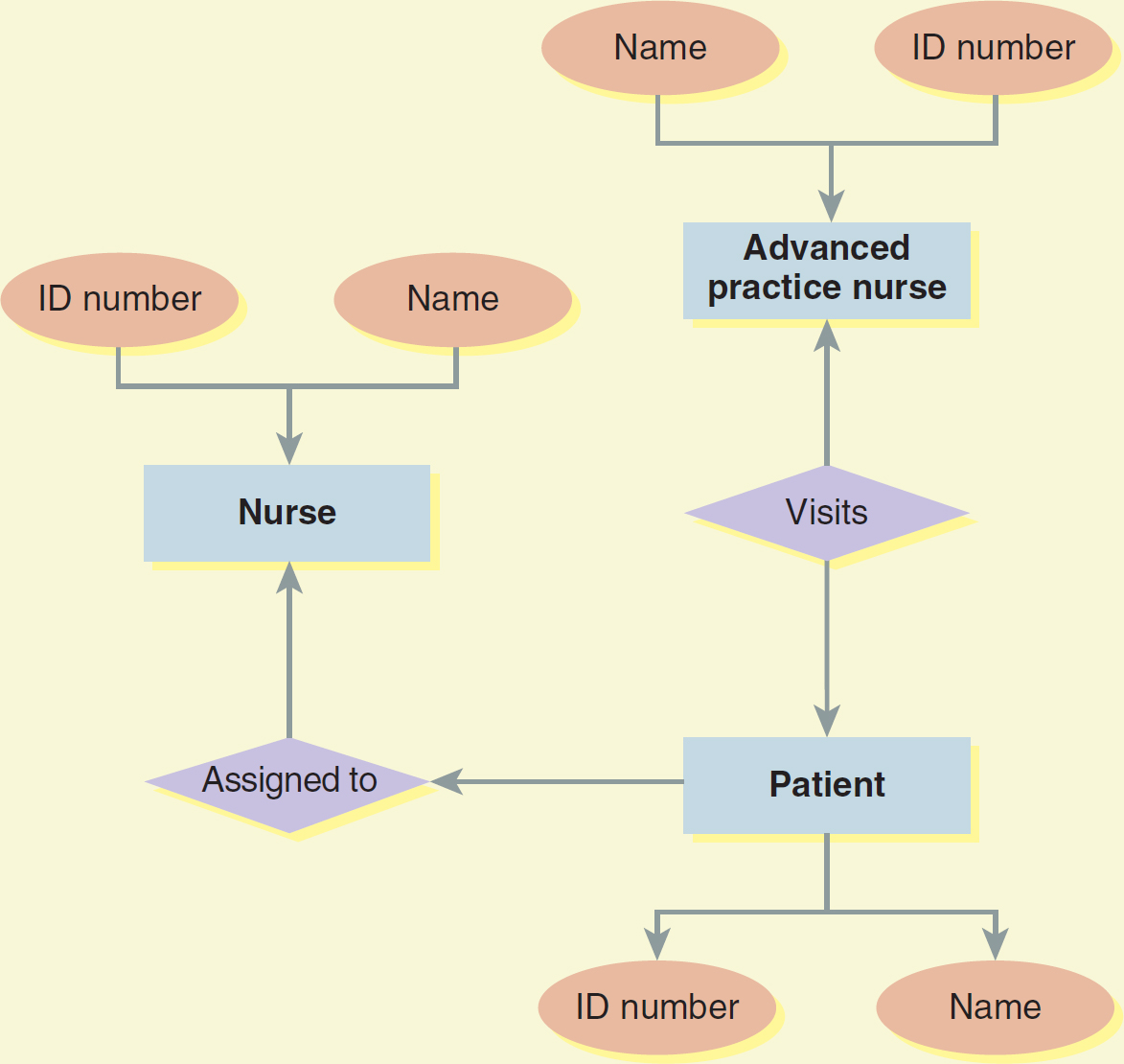
The entity relationship diagram specifies the relationship among the entities in the database. Sometimes the implied relationships are readily apparent based on the entities' definitions; however, all relationships should be specified as to how they relate to one another. Typically, three relationships are possible: (1) one to one, (2) one to many, and (3) many to many. A one-to-one relationship exists between the entities of the table about a patient and the table about the patient's birth. A one-to-many relationship could exist when one entity is repeatedly used by another entity. Such a one-to-many relationship could then be a table query for age that could be used numerous times for one patient entity. The many-to-many relationship reflects entities that are used repeatedly by other entities. This is easily explained by the entities of patient and nurse. The patient could have several nurses caring for them, and the nurse could have many patients assigned to them (see Figure 10-2).
Figure 10-2 Example of an Entity Relationship Diagram
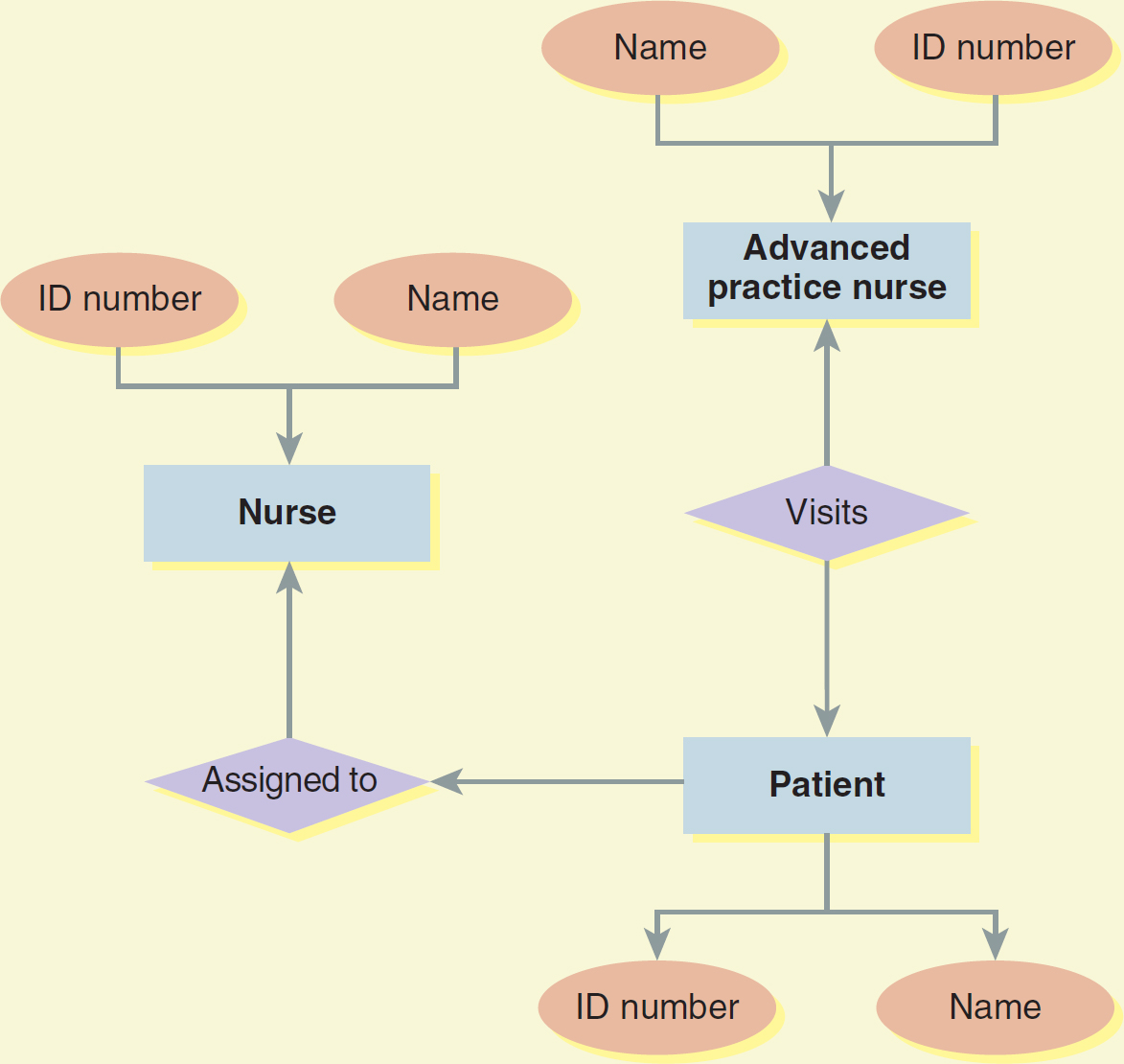
A flowchart depicts the interaction between an advanced practice nurse, a nurse, and a patient.
The flow begins with the identification of the advanced practice nurse, including their name and I D number. Subsequently, a patient, identified by name and I D number, visits the advanced practice nurse. The flow also indicates the assignment of the patient to the nurse, with the nurse's name and I D number included in this process.
The relational model is a database model that describes data in which all data elements are placed in relation in two-dimensional tables; the relations, or tables, are analogous to files. A relational database management system (RDMS) is a system that manages data using this kind of relational model. A relational database could link a patient's table to a treatment table (e.g., by a common field, such as the patient ID number). To keep track of the tables that constitute a database, the database management system uses software called a data dictionary. The data dictionary contains a listing of the tables and their details, including field names, validation settings, and data types. The data type refers to the type of information, such as a name, a date, or a time.
The database management system is an important program because, before it was available, many health systems and businesses had dozens of database files with incompatible formats. Because patient data come from a variety of sources, these separated, isolated data files required duplicate entry of the same information, thereby increasing the risk of data entry error. The design of the relational databases eliminates data duplication. Some examples of popular database management system software include Microsoft's Access and Visual FoxPro, Oracle's Oracle Database 21c, and IBM's Db2.
|
On a large scale, a data warehouse is an extremely large database, or repository, that stores all of an organization's or institution's data and makes these data available for data mining. The data warehouse can combine an institution's many databases to provide management personnel with flexible access to the data. On a smaller scale, a data mart represents a large database in which the data used by one of the units or a division of a healthcare system are stored and maintained. For example, a university hospital system might store clinical information from its many affiliate hospitals in a data warehouse, and each separate hospital might have a data mart housing its data.
There are many ways to access and retrieve information in databases. Searching information in databases can be done through the use of a query, as is used in Microsoft's Access database. A query asks questions of the database to retrieve specific data and information. Box 10-2 provides a detailed description of the Structured Query Language (SQL).
| Box 10-2 Structured Query Language (SQL) |
|---|
| SQL was originally called SEQUEL, or Structured English Query Language. SQL, still pronounced “sequel,” now stands for Structured Query Language; it is a database querying language, rather than a programming language, and a standard language for accessing and manipulating databases. SQL is “used with relational databases; it allows users to define the structure and organization of stored data, verify and maintain data integrity, control access to the data, and define relationships among the stored data items” (Blink, 2016, para. 8). SQL simplifies the process of retrieving information from a database in a functional or usable form while facilitating the reorganization of data within the databases.
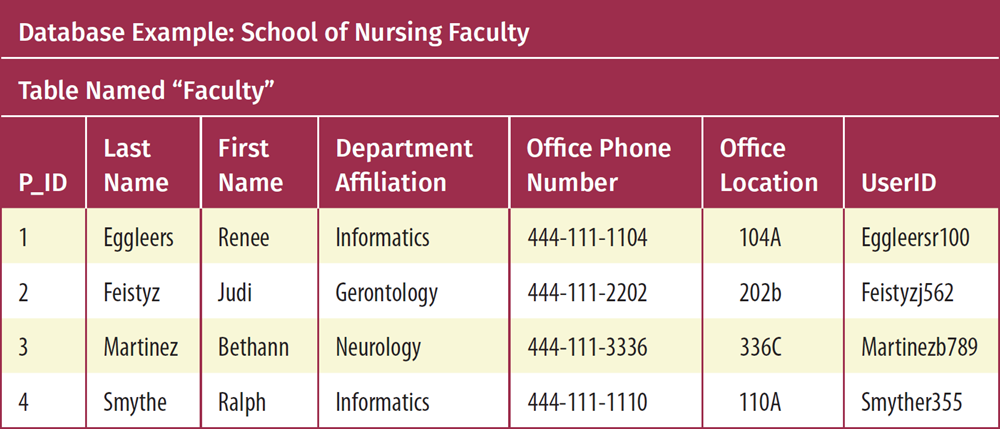
The RDMS is the foundation for SQL. Data in an RDMS are stored in tables. A table is a collection of related data that consists of columns, which are also referred to as fields, and rows, which are also referred to as records, or tuples (Peterson, 2023). Databases can have many tables, and each table is identified by a name. The consistent formatting and organization of data in an RDMS allows a user to easily enter, view, and manipulate data (see the following Database Example: School of Nursing Faculty).
SQL statements handle most of the actions users need to perform on a database. SQL is an International Organization for Standardization (ISO) and American National Standards Institute (ANSI) standard (Indiana University, 2021). To remain compliant with the ISO and ANSI standards, SQL must handle or support the most typical major commands such as SELECT, UPDATE, DELETE, INSERT, and WHERE (Prateek, 2023). The SELECT command allows extraction of data from a database, UPDATE updates the data, DELETE deletes the data, and INSERT inserts new data. WHERE is used to specify selection criteria, thereby restricting the results of the SQL query. Thus, SQL allows the creation of databases and their manipulation by storing, retrieving, updating, and deleting data. Coursera (2023) described SQL as a powerful method of storing and being able to interact with data. SQL supports high-quality data analysis due to its flexibility and power.
|
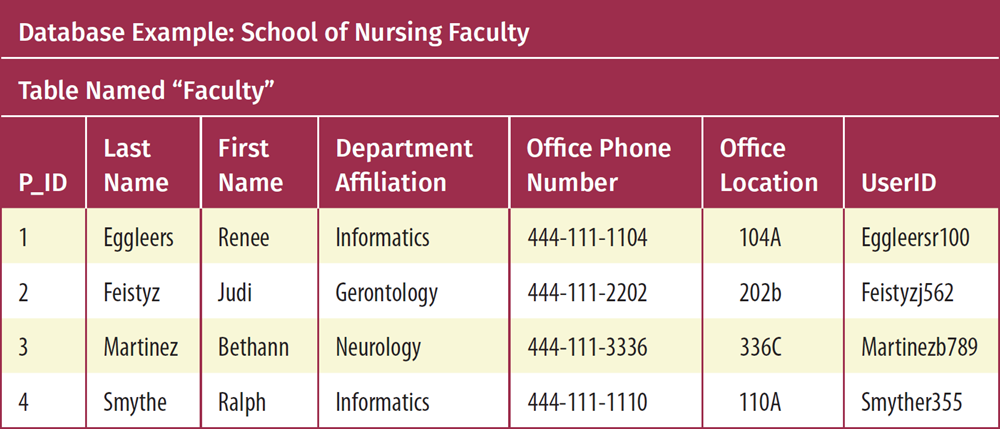 Box titled: Structured Query Language, S Q L, continued. The text continues as follows. The database example provided here reflects the faculty listing for a school of nursing. The table that contains the data is identified by the name, Faculty. The faculty members are categorized by the following fields, columns: Last Name, First Name, Department Affiliation, Office Phone Number, Office Location, and User I D. Each faculty member's information is a record, tuple, or row. Using the S Q L command SELECT, all the records in the, Faculty, table can be selected: SELECT, asterisk FROM Faculty This command would SELECT all, asterisk, of the records FROM the table known as FACULTY. The asterisk, asterisk, is used to select all the columns. The database example provided here reflects the faculty listing for a school of nursing. The table that contains the data is identified by the name “Faculty.” The faculty members are categorized by the following fields (columns): Last Name, First Name, Department Affiliation, Office Phone Number, Office Location, and UserID. Each faculty member's information is a record (tuple, or row). Using the SQL command SELECT, all the records in the “Faculty” table can be selected: |
This command would SELECT all (*) of the records FROM the table known as FACULTY. The asterisk (*) is used to select all the columns. |
Data mining software sorts through data to discover patterns and ascertain relationships. This software discovers previously unidentified relationships among the data in a database by conducting an exploratory analysis looking for hidden patterns in data. Using such software, the user searches for previously undiscovered patterns by analyzing the data stored in a data warehouse. Drill down is a term that means the user can view data warehouse information by drilling down to lower levels of the database to focus on information that is pertinent to their needs at the moment.
As users move through databases within the healthcare system, they can access anything from enterprise-wide data warehouses to data marts. For example, an infection control nurse might notice a pattern of methicillin-resistant Staphylococcus aureus infections in the local data mart (a single hospital within a larger system). The nurse might want to find out whether the outbreak is local (data mart) or more widespread in the system (data warehouse). The nurse might also query the database to determine whether certain patient attributes (e.g., age or medical diagnosis) are associated with the incidence of infection.
These kinds of data mining capabilities are also quite useful for healthcare practitioners who wish to conduct clinical research studies. For example, one might query a database to tease out attributes (i.e., patient characteristics) associated with asthma-related hospitalizations.
In 2013, Mishra et al. were the first to report on a new set of challenges and opportunities for managing data and data mining and establishing data analysis algorithms in the cloud. At the time, this development was game changing for organizations. The world as we knew it was changing. Clouds are leading us to develop revolutionary data mining technologies because the organization can take advantage of the sophisticated software and processing methodology available from the cloud provider without having to invest in them individually. Hein (2019) discussed the benefits and risks of cloud computing in health care. Benefits include data storage capacity, scalability (i.e., matching service demands), ease of collaboration, and access to AI and machine learning processing. Risks include training needed for proper implementation, security vulnerabilities, HIPAA compliance, and availability and control of the data.
Blockchain technology is showing great promise in solving some of the issues associated with traditional databases and cloud computing. Blockchain is widely described as a distributed ledger technology. “A blockchain is, in the simplest of terms, a time-stamped series of immutable record of data that is managed by a cluster of computers not owned by any single entity. Each of these blocks of data (i.e., block) is secured and bound to each other using cryptographic principles (i.e., chain)” (Chadha, 2020, para. 7). Every transaction is recorded in the blockchain and trackable, and authorized users will have immediate access to records updated in real time. However, each new change is recorded in a new block so that authorized users can retrace the steps in the information trail to understand changes as they occurred. These private chains are also referred to as permissioned chains, and they offer a high level of security. Potential uses of blockchain technology in health care include managing patient records with a hash ID unique identifier to allow more accurate matching of records from different providers, seamless sharing of records and health data as the patient permits, incentivizing healthy behaviors, managing the pharmacy supply chain, curtailing insurance fraud, and conducting research and clinical trials using secure and trusted data (Chadha, 2020). Block chain is currently being used in health care for “everything from securing patient data to managing the pharmaceutical supply chain” (Daley, 2023, para. 1).
Department Collaboration and Exchange of Knowledge and Information ⬆ ⬇
The implementation of systems within health care is the responsibility of many people and departments. All systems require a partnership of collaboration and knowledge sharing to implement and maintain successful standards of care. Collaboration is the sharing of ideas and experiences for the purposes of mutual understanding and learning. Knowledge exchange is the product of collaboration when sharing an understanding of information promotes learning from past experiences to make better future decisions.
Depending on the type of project, collaboration may occur at several levels within an organization. At an administrative level, collaboration among key stakeholders is critical to the success of any project. Stakeholders have the most responsibility for completing the project. They have the greatest influence on the overall design of the system because, ultimately, they are the people who are most impacted by a system implementation. Together with the organizational executive team, stakeholders collaborate on the overall budget and time frame for a system implementation.
Collaboration may also occur among the various departments affected by the system. These groups frequently include representatives from IT, clinical specialty areas, support services, and software vendors. Once a team is assembled, it defines the objectives and goals of the system. The team members work strategically to align their goals with the goals of the organization where the system is to be used. The focus for these groups is on planning, resource management, transitioning, and ongoing support of the system. Their collaboration determines the way in which the project is managed-the deliverables for the project, the individuals held accountable for the project, the time frame for the project, and the opportunities for process improvement using the system-and the means by which resources are allocated to support the system.
From collaboration comes the exchange of information and ideas through knowledge sharing. Specialists exchange knowledge within their respective areas of expertise to ensure that the system works for an entire organization. From one another, they learn the requirements that make the system successful. This exchange of ideas is what makes healthcare ISs so valuable. A multidisciplinary approach ensures that systems work in the complex environment of healthcare organizations, which have diverse and complex patient populations.
Summary ⬆ ⬇
The integration of technology within healthcare organizations offers limitless possibilities. As new types of systems emerge, clinicians will become smarter and more adept at incorporating these tools into their daily practice. Success will be achieved when health care incorporates technology systems in a way that they are not viewed as separate tools to support healthcare practices but rather as necessary instruments to provide healthcare. Patients, too, will become savvier at using healthcare ISs as a means of communicating and managing their personal and preventive care. In the future, these two mindsets will become expectations for health care and not simply a high-tech benefit, as they are often viewed today.
Ultimately, it is not the type of systems adopted that is important but rather the method in which they are put into practice. In an ideal world, robust and transparent information technologies will support clinical and administrative functions and promote safe, high-quality, and cost-effective care.
| Thought-Provoking Questions |
|---|
- Which type of technology exists today that could be converted into new types of ISs to be used in health care?
- How could collaboration and knowledge sharing at a single organization be used to help individuals preparing for IT at a different facility?
- Explore the administrative ISs and their applications in your healthcare organization.
- What are the main systems used?
- How are data shared among systems?
- What examples of functional, structural, and semantic interoperability can you identify?
- Reflect on the communication tools available in a clinical setting. How do UC systems affect and address the inefficiencies in communication that currently exist? What else needs to be done to eliminate communication inefficiency and gaps?
- Assess all the reasons, in detail, as to why CDI is necessary. How does it address missing, incomplete, and inaccurate records, including coding errors? Could AI be employed to complete this task? Explain, in detail, why or why not.
- Why are ADT systems critical to the improvement of communication across care providers? How can ADT improve chronic care patient management and reduce unnecessary hospital utilization?
|
References ⬆
- AAPC. (2023). What is clinical documentation improvement?www.aapc.com/resources/what-is-clinical-documentation
- Agarwal R., Sands D., Schneider J., & Smaltz D. (2010). Quantifying the economic impact of communication inefficiencies in U.S. hospitals. Journal of Healthcare Management, 55(4), 265-281.
- Agency for Healthcare Research and Quality Patient Safety Network. (2019). Patient safety primer: Medication errors and adverse drug events. https://psnet.ahrq.gov/primer/medication-errors-and-adverse-drug-events
- AHIMA. (2020). Ethical standards for clinical documentation integrity (CDI) professionals (2020).www.ahima.org/media/r2gmhlop/ethical-standards-for-clinical-documentation-integrity-cdi-professionals-2020.pdf?oid=301868
- Blink. (2016, April 28). Data warehouse terms.University of California at San Diego. https://blink.ucsd.edu/technology/help-desk/queries/warehouse/terms.html
- Brink J., Arenson R., Grist T., Lewin J., & Enzmann D. (2017). Bits and bytes: The future of radiology lies in informatics and information technology. European Radiology, 27(9), 3647-3651. https://doi.org/10.1007/s00330-016-4688-5
- Carter R. (2022, January 17). The state of unified communications in healthcare 2022. UC Today. www.uctoday.com/unified-communications/the-state-of-unified-communications-in-healthcare-2022
- Centers for Medicare and Medicaid Services. (2020). Accountable care organizations (ACOs). www.medicare.gov/manage-your-health/coordinating-your-care/accountable-care-organizations
- Chadha B. (2020, April 24). The true importance of blockchain education. Blockgeeks. https://blockgeeks.com/guides/blockchain-education
- Coursera. (2023, June 16). SQL vs. MySQL: Differences, similarities, uses, and benefits.www.coursera.org/articles/sql-vs-mysql
- Daley S. (2023, February 16). Blockchain in healthcare: 17 Examples to know 2023. Built In. https://builtin.com/blockchain/blockchain-healthcare-applications-companies
- Davis E. (2022, March 10). Duties and types of case managers. Verywell Health. www.verywellhealth.com/what-does-a-case-manager-do-1738560
- DeGaspari J. (2013, September 11). Data storage strategies: Not all in the cloud. Healthcare Innovation. www.hcinnovationgroup.com/interoperability-hie/infrastructure/article/13021976/data-storage-strategies-not-all-in-the-cloud
- DeLeon H. (n.d.). Enterprise resource planning in the healthcare industry. Hospital Jobs Online. www.hospitaljobsonline.com/career-center/healthcare-careers/enterprise-resource-planning-in-the-healthcare-industry.html
- Dinsdale E., Hannigan A., O'Connor R., O'Doherty J., Glynn L., Casey M., Hayes P., Kelly D., Cullen W., & O'Regan A. (2020). Communication between primary and secondary care: Deficits and danger. Family Practice, 37(1), 63-68. https://doi.org/10.1093/fampra/cmz037
- Fichman R. G., Kohli R., & Krishnan R. (2011). Editorial overview-The role of information systems in healthcare: Current research and future trends. Information Systems Research, 22(3), 419-428. https://doi.org/10.1287/isre.1110.0382
- Fico G., Fioravanti A., Arredondo M. T., Gorman J., Diazzi C., Arcuri G., Conti C., & Pirini G. (2016). Integration of personalized healthcare pathways in an ICT platform for diabetes managements: A small-scale exploratory study. IEEE Journal of Biomedical and Health Informatics, 20(1), 29-38. http://dx.doi.org/10.1109/JBHI.2014.2367863
- Futrell K. (2021, February 22). COVID-19 highlights need for laboratory data sharing and interoperability. Medical Laboratory Observer. www.mlo-online.com/information-technology/lis/article/21210723/covid19-highlights-need-for-laboratory-data-sharing-and-interoperability
- Gilbert J., Helfand M., & Relevo R. (2018). High utilizers of healthcare. https://effectivehealthcare.ahrq.gov/system/files/docs/topic-brief-high-utilizers.pdf
- Glickman M., & Orlova A. (2022). Building interoperability standards and ensuring patient safety. AHIMA. https://bok.ahima.org/doc?oid=107799-.Y-AF7y_MK3A
- Gordon C. R., Rezzadeh K. S., Li A., Vardanian A., Zelken J., Shores J. T., Sacks J. M., Segovia A. L., & Jarrahy R. (2015). Digital mobile technology facilitates HIPAA-sensitive perioperative messaging, improves physician-patient communication, and streamlines patient care. Patient Safety in Surgery, 9(1), 1-7. http://dx.doi.org/10.1186/s13037-015-0070-9
- Halvorsen D. (2018). Technology expansion. State of Pharmacy Automation, 15(8), 4. www.pppmag.com/article/2260
- Handzel S. (2021, May 10). How one hospital changed nurse staffing models in response to COVID-19. Wolters Kluwer. www.wolterskluwer.com/en/expert-insights/how-one-hospital-changed-nurse-staffing-models-in-response-to-covid
- Healthcare Information and Management Systems Society. (n.d.). Interoperability in healthcare. www.himss.org/resources/interoperability-healthcare
- HealthShare Exchange. (n.d.). Hospitals & health systems. www.healthshareexchange.org/hospitals-health-systems
- Hein D. (2019, January 22). 8 Benefits and risks of cloud computing in healthcare. Solutions Review. https://solutionsreview.com/cloud-platforms/8-benefits-and-risks-of-cloud-computing-in-healthcare
- IEEE Standards Association. (2023, January 11). How can standards help monitor our health and wellness?https://standards.ieee.org/beyond-standards/how-can-standards-help-monitor-our-health-and-wellness
- IEEE Standards University. (2016, September 23). Standards glossary. www.standardsuniversity.org/article/standards-glossary
- Indiana University. (2021, September 20). SQL example statements for retrieving data from a table. http://kb.iu.edu/data/ahux.html
- Institute of Medicine. (2000). To err is human: Building a safer health system. National Academies Press.
- Kholodenko O. (2022, November 16). Data storage in healthcare. CodeIT. https://codeit.us/blog/data-storage-in-healthcare
- MarketWatch. (2023, June 5). Robotic prescription dispensing systems market research 2023-2030 [Press release]. www.marketwatch.com/press-release/robotic-prescription-dispensing-systems-market-research-2023-2030-2023-06-05
- Maruster L., van der Zee , D-J., & Buskens E. (2021). Identifying frequent health care users and care consumption patterns: Process mining of emergency medical services data. Journal of Medical Internet Research, 23(10), e27499. doi:10.2196/27499
- MerlinOne. (n.d.). What is metadata tagging?https://merlinone.com/what-is-metadata-tagging.
- Michigan Health Information Network. (n.d.). Admission, discharge, transfer notifications (ADT) use case.https://mihin.org/admission-discharge-transfer-notifications-use-case
- Michigan Health Information Network. (2019, May 9). Admission, discharge, transfer notifications: Implementation guide. https://mihin.org/wp-content/uploads/2019/05/Microsoft-Word-MiHIN-UCIG-ADT-Notifications-v46-05-09-19.pdf
- Miliard M. (2017, September 27). How to improve clinical documentation. Healthcare IT News. www.healthcareitnews.com/news/how-improve-clinical-documentation
- Miller R. (2023). MCG chronic care guidelines. MCG Health. www.mcg.com/care-guidelines/chronic-care
- Mishra N., Sharma S., & Pandey A. (2013). High performance cloud data mining algorithm and data mining in clouds. IOSR Journal of Computer Engineering, 8(4), 54-61. https://pdfs.semanticscholar.org/2d03/59258ed04703fd03d8e878527442d61939b6.pdf
- Mock T. (2021, March 31). What are common communication systems in healthcare? Rave Mobile Safety. www.ravemobilesafety.com/blog/common-communication-systems-healthcare
- Muin M. (2017, April 23). What are the uses and benefits of a laboratory information system? MedProjects. http://medprojects.com/2017/what-are-the-uses-and-benefits-of-a-laboratory-information-system
- Office of the National Coordinator for Health Information Technology. (2013, May). Improving hospital transitions and care coordination using automated admission, discharge and transfer alerts: A learning guide. www.healthit.gov/sites/default/files/onc-beacon-lg1-adt-alerts-for-toc-and-care-coord.pdf
- Office of the National Coordinator for Health Information Technology. (2015). Connecting health and care for the nation: A shared nationwide interoperability roadmap. www.healthit.gov/sites/default/files/hie-interoperability/nationwide-interoperability-roadmap-final-version-1.0.pdf
- Peterson R. (2023, July 20). Difference between DBMS and RDBMS. Guru99. www.guru99.com/difference-dbms-vs-rdbms.html
- Phamily. (n.d.). The #1 text-based chronic care management software.https://join.phamily.com/ccm-solution
- Ponemon Istitute. (2014, June). The Imprivata report on the economic impact of inefficient communications in healthcare. www.ponemon.org/local/upload/file/2014%20Imprivata%20Report%20FINAL%203(1).pdf
- Posnack S. (2021a, May 13). Health interoperability outcomes 2030. Heath IT Buzz. www.healthit.gov/buzz-blog/interoperability/health-interoperability-outcomes-2030
- Posnack S. (2021b, May 4). A road well traveled - Sunsetting the interoperability roadmap. Health IT Buzz. www.healthit.gov/buzz-blog/health-it/a-road-well-traveled-sunsetting-the-interoperability-roadmap
- Prateek T. L. (2023, June 19). SQL basics - One stop solution for beginners. Edureka! www.edureka.co/blog/sql-basics
- Rockall A. (2019). From hype to hope to hard work: Developing responsible AI for radiology. Clinical Radiology, 75(1), 1-2. http://dx.doi.org/10.1016/j.crad.2019.09.123
- SmartData Collective. (2015, October 5). Two critical obstacles facing retailers for data driven marketing. www.smartdatacollective.com/two-critical-obstacles-facing-retailers-data-driven-marketing
- Trepanier S., Lee D. W., & Kerfoot K. M. (2017). Interoperable acuity-based staffing solutions: Lessons learned from a multi-hospital system. Nursing Economics, 35(4), 184-188, 204.
- Tsai M., Xirasagar S., Carroll S., Bryan C., Gallagher P., Davis K., & Jauch E. (2018). Reducing high-users' visits to the emergency department by a primary care intervention for the uninsured: A retrospective study. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55, 004695801876397.
- Wong C. (2022, June 7). The importance of an ADT message system. Experience.care. https://experience.care/blog/importance-of-an-adt-message-system