Objectives ⬇
- Provide an overview of the purpose of conducting workflow analysis and design.
- Deliver specific instructions on workflow analysis and redesign techniques.
- Cite measures of efficiency and effectiveness that can be applied to redesign efforts.
- Explore quality improvement processes.
Key Terms ⬆ ⬇
Introduction ⬆ ⬇
The healthcare environment has grown more complex over the years and continues to evolve every day. Unfortunately, the complexities that help clinicians deliver better care and improve patient outcomes also take a toll on the clinicians themselves. This toll is exemplified through hours spent learning new technology, loss in productivity as users adjust and adapt to new technology, and unintended workflow consequences from the use of technology.
Despite the perceived negative downstream effects to end users and patients as a result of technology, this very same technology can improve efficiency and yield a leaner healthcare environment. The intent of this chapter is to outline the driving forces that create the need to manage or redesign workflow as well as elucidate what the nurse must know about how to conduct workflow redesign, measure the effect of workflow changes, and promote the best use of technology.
Purpose of Workflow Analysis ⬆ ⬇
According to The Patient Safety League (2023), “2.2 million patients are harmed by medical errors every day in this country and 440,000 of them DIE from PREVENTABLE medical errors daily.”
Not only is there an effect on patients and their families from these errors but also there is a significant financial effect on healthcare organizations. Clearly, we must minimize these errors, and one of the most important tools for this purpose is the use of electronic health records and information systems to improve communication and provide point-of-care decision support and automation.
Technology can provide a mechanism to improve care delivery and create a safer patient environment provided it is implemented appropriately and considers the effect on the surrounding workflow. In an important early article, Campbell et al. (2009) suggested that technology implemented without consideration of user workflow can create greater patient safety concerns than no technology at all. Consideration of computerized provider order entry (CPOE), for example, helps us to focus more specifically on workflow effects. Sometimes these negative workflow implications are referred to as the unintended consequences of CPOE implementation and were likely due to poorly implemented technology. Ash et al. (2009) reported on nine unintended consequences of CPOE. Interestingly, a later study by Abraham et al. (2018) also reported on workflow process issues with CPOE, and they identified four core categories: order entry issues, user issues, system limitations, and care transition issues.
The Healthcare Information Management Systems Society Toolkit addressed workflow redesign and considered why it is so critical to successful technology implementations. Replacing or upgrading a system that was already automated requires substantially less workflow redesign than implementing an information technology (IT) system that addresses a process that was not previously automated. The toolkit was instrumental in identifying and describing several workflow improvement theories. These theories and others are still used today: total quality management (TQM), business process reengineering (BPR), plan-do-check-act (PDCA), Six Sigma, Lean and Lean Six Sigma, business process management (BPM), and five whys analysis (Laoyan, 2023). Consistently and rigorously using these theories helps support process improvements in an organization by providing well-defined processes and improved workflows. Reflect on the addition of machine learning and artificial intelligence (AI) (Health Catalyst, 2021; Hopkins, 2019). For more information about each of these processes, review the information provided in the cited references, or search for each one individually.
Nursing informaticists are invaluable for successful system implementation by defining clinical workflow, enhancing efficiencies, improving quality, and acting as change agents to promote adoption (Schoenbaum & Carroll, 2021). Thompson et al. (2016) stated that “[b]y partnering clinicians with informaticists we strove to leverage the power of the electronic medical record (EMR) to reduce heart failure readmissions and improve patient transitions back to the community” (p. 380). They concluded that “[p]artnering with clinical informatics enabled the multidisciplinary team to leverage the power of the EMR in supporting and tracking new clinical workflows that impact patient outcomes” (p. 380). This multidisciplinary team believed that its success could reshape how healthcare providers facilitate patient discharge and the transition home. Leveraging the multidisciplinary team and the EMR could provide a model for patient-centered and cost-effective care that could extend beyond its patients with heart failure.
Technology is recognized to have a potentially positive effect on patient outcomes. Nevertheless, even with the promise of improving how care is delivered, adoption of technology was slow. The cost of technology solutions, such as CPOE, barcode medication administration, and electronic health records (EHRs), was one of the main reasons for initial resistance. The cost of technology, coupled with the lengthy timelines required to develop and implement such technology, initially put this endeavor out of reach for many healthcare organizations. In addition, upgrades to the technology are often necessary either during the implementation or shortly after a launch, leaving little time to focus efforts on the optimization of the technology within the current workflow. Furthermore, the existence of technology does not in itself guarantee that it will be used in a manner that promotes better outcomes for patients.
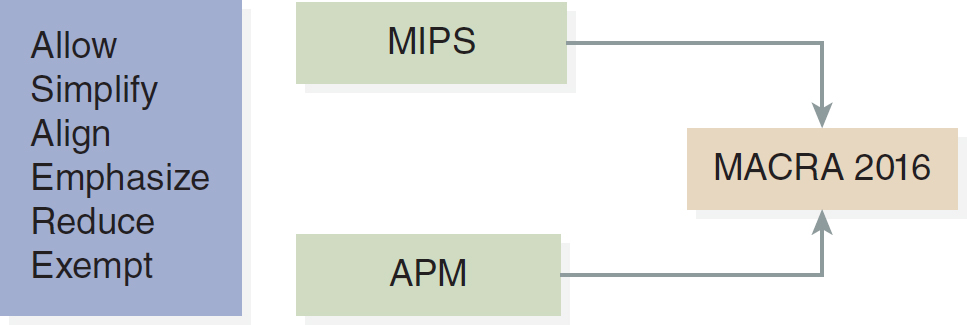
Given the sluggish adoption of technology, in 2009 the U.S. government took an unprecedented step when it formally recognized the importance of health information technology for patient care outcomes. As a result of the provisions of the American Recovery and Reinvestment Act (ARRA), healthcare organizations were able to qualify for financial incentives based on the level of meaningful use achieved. Meaningful use referred to the rules and regulations established by the ARRA. The three stages of meaningful use were part of an EHR incentive program, renamed in 2018 to Promoting Interoperability Programs (Centers for Medicare and Medicaid Services [CMS], 2022). During stage 1, the focus was on data capturing and sharing. Stage 2 focused on advanced clinical processes, and stage 3 sought to improve outcomes. Stage 1 was initiated from 2011 to 2012, stage 2 began in 2014, and stage 3 was established in 2017 (CMS, 2021). However, with the new goal of paying for value and better care, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) reformed Medicare payments by making changes that created the Quality Payment Program to replace the hodgepodge system of Medicare reporting programs (CMS, 2016b; see Figure 13-1). The MACRA Quality Payment Program has two paths-Merit-based Incentive Payment System (MIPS) or Alternative Payment Model (APM)-which will be in effect through 2021 and beyond (CMS, 2016b). The MACRA requirements for the Measure Development Plan follow:
Figure 13-1 MACRA
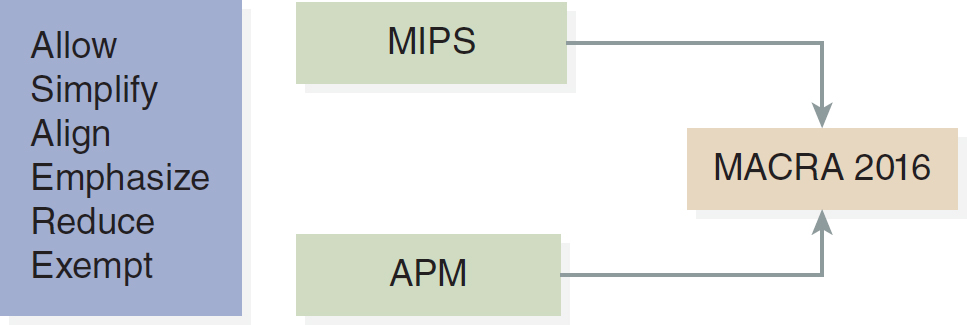
A flow diagram depicts M A C R A 2016 act, encompassing M I P S and A P M. The diagram includes key actions such as allow, simplify, align, emphasize, reduce, and exempt.
- Multipayer applicability
- Coordination and sharing across measure developers
- Clinical practice guidelines
- Evidence base for nonendorsed measures
- Gap analysis
- Quality domains and priorities
- Applicability of measures across healthcare settings
- Clinical practice improvement activities
- Considerations for electronic specifications and Qualified Clinical Data Registries (QCDRs) (CMS, 2016a, p. 16)
For an organization seeking to meet these measures, the data to support these measures must be gathered and reported on electronically, which necessitates the use of technology in all patient care areas. The successful implementation of the Measurement Development Plan “depends on a successful partnership with patients, frontline clinicians, and professional organizations and collaboration with other diverse stakeholders to develop measures that are meaningful to patients and clinicians and can be used across payers and health care settings” (CMS, 2016a, p. 64). Many of the quality reporting measures rely on nursing and medical documentation. Most healthcare personnel already use EHRs, but MACRA measures pushed healthcare organizations to reexamine the use of clinical technologies within their organizations and approach implementation in a new way.
Not only is there a potential for patient safety and quality issues to arise from technology implementation that does not address workflow, but a financial impact on the organization is possible as well. We must make sure that technology is not a barrier to quality healthcare and patient safety (American Society for Health Care Risk Management [ASHRM], 2021). All organizations, regardless of their industry, must operate efficiently to maintain profits and continue to provide services to their customers. For hospitals, which normally have significantly smaller profit margins than other organizations, the need to maintain efficient and effective care is essential for survival. Given that hospital profit margins are diminishing, never has there been a more crucial time than now to examine the costs of errors and poorly designed workflows and the financial burden they present to an organization. Moreover, what are the costs to an organization that fails to address the appropriate integration of technology? This is an area for which few supporting data exist to substantiate the claim that technology without workflow considerations can, in fact, affect the bottom line.
Many healthcare organizations have or are still experiencing the effects of poorly implemented clinical technology solutions. These effects may be manifested in the form of redundant documentation, non-value-added steps, and additional time spent at the computer rather than in direct care delivery. Consider these post-implementation examples of workflow issues. Gugerty et al. (2007) studied the challenges and opportunities in nursing documentation and determined that it was possible to decrease by 25% per shift the time a nurse spends documenting. Technology ought not to be implemented for the sake of automation unless it promises to deliver gains in patient outcomes and proper workflow. In fact, the cost to organizations for duplicate/redundant documentation by nursing can range from $6,500 to $13,000 per nurse per year (Clancy et al., 2006). Stokowski (2013) found other issues, such as systems that are slow and freeze; lose data; and “don't dump data from monitors and screening devices into the EHR in real time,” which slows the documentation process and increases the amount of time the nurse must spend on the computer and not in direct patient care (p. 9). Cision PR Newswire (2018) reported on a Black Book Market Research survey that 96% of nurse survey respondents are largely satisfied with EHR documentation and 83% appreciated the quick responses by IT departments to reported issues. On a positive note, “[e]ighty-five percent of nurses now see competency with at least one EHR as a highly-sought employment skill for an RN, and sixty-five percent believe nurses with multiple fluencies are deemed a highly superior job candidate currently by health systems” (para. 9). However, there are still some challenges negatively affecting workflow because computers or handheld devices are not in every room.
Examining the workflow surrounding the use of technology enables better use of the technology and more efficient work. It also promotes safer patient care delivery. The need to focus on workflow and technology is attracting increasing recognition, although a dearth of literature remains that addresses the importance of this area. As more organizations work to achieve a level of technology adoption that will enable them to meet MACRA measures and receive financial payments, more attention will be paid to the area of workflow design, resulting in a greater body of research and evidence (Agency for Healthcare Research and Quality [AHRQ], n.d.; Yuan et al., 2013).
Workflow and Technology ⬆ ⬇
Workflow is a term used to describe the action or execution of a series of tasks in a prescribed sequence. Another definition of workflow is a progression of steps (i.e., tasks, events, or interactions) that constitute a work process, involve two or more persons, and create or add value to the organization's activities. In a sequential workflow, each step depends on the occurrence of the previous step; in a parallel workflow, two or more steps can occur concurrently. Sometimes the term workflow is used interchangeably with process or process flows, particularly in the context of implementations. Observation and documentation of workflow to better understand what is happening in the current environment and how it can be altered is referred to as workflow analysis. A typical output of workflow analysis is a visual depiction of the process, called a process map. The process map ranges from simplistic to fairly complex and provides an excellent tool for identifying specific steps. It can also provide a vehicle for communication and a tool upon which to build educational materials as well as policies and procedures.
One school of thought suggests that technology should be designed to meet the needs of clinical workflow (Yuan et al., 2013). This model implies that system analysts have a high degree of control over screen layout and data capture. It also implies that technology is malleable enough to allow for the flexibility to adapt to a variety of workflow scenarios. Lessons learned from more than three decades of clinical technology implementations suggest that clinical technologies still have a long way to go on the road to maturity to allow this to be possible. The second and probably most prevalent thought process is that workflow should be adapted to the use of technology. Today, this is by far the most commonly used model given the progress of clinical technology. Bucur et al. (2016) developed clinical models to support clinical decision-making that were inserted into the workflow models. This system integrates a workflow suite and functionality for the storage, management, and execution of clinical workflows and the storage of traces of execution. The knowledge models are integrated and run from the workflow to support decisions at the right point in the clinical process (Bucur et al., 2016, p. 152). The ability to track and assess decision-making throughout a clinical course of care for a patient will enhance nursing knowledge and improve patient care. Flohr et al. (2018) described a design process for a mobile application that would combine outputs from multiple pieces of intensive care unit equipment to aid clinicians in assessing, processing, and clinical decision-making. Their approach included 54 hours of clinical observations as well as stakeholder interviews. In this way, workflow informed the technology design rather than the technology driving the consequent workflow.
A concept that has gained popularity in recent years relative to workflow redesign is clinical transformation. Clinical transformation is the complete alteration of the clinical environment; therefore, this term should be used cautiously to describe redesign efforts. Earl et al. (1995) defined transformation as “a radical change approach that produces a more responsive organization that is more capable of performing in unstable and changing environments that organizations continue to be faced with” (p. 31). Many workflow redesign efforts are focused on relatively small changes and not on the widespread change that accompanies transformational activities. Moreover, clinical transformation would imply that the manner in which work is carried out and the outcomes achieved are completely different from the prior state, which is not always true when the change simply involves implementing technology. Technology can be used to launch or in conjunction with a clinical transformation initiative, although the implementation of technology alone is not perceived as transformational.
Before undertaking transformative initiatives, the following guidelines should be understood:
- Leadership must take the lead and create a case for transformation.
- Establish a vision for the end point.
- Allow those persons with specific expertise to provide the details.
- Think about the most optimal experience for both the patient and the clinician.
- Do not replicate the current state.
- Focus on those initiatives that offer the greatest value to the organization.
- Recognize that small gains have no real impact on transformation.
Holston (2022) reported on Patient Room ‘Next' (PRN), which is an approach to provide high-quality health care to patients wherever they are located. The patient could be in the community, their home, or even an ambulance. The PRN strategy looks to the future of technology and patient care in five key categories: “machine vision, machine audio, content interaction with patients, sensors and telehealth” (para. 3). There is a need to improve patient care and clinical workflows through the five goals of the PRN: (1) the easy button, (2) real-time data knowledge, (3) automated documentation, (4) touchless technology, and (5) flexible spaces (Holston, 2022). The easy button refers to access to patient data and information for the clinicians when they need it. Real-time data knowledge provides the best data and information possible at the time of care so that the clinicians can make informed diagnoses and decisions. Automated documentation allows the clinicians to spend less time in the EHR and more time with their patients. Touchless technology uses equipment such as cameras and sensors to monitor the patient without disturbance. Flexible spaces allow healthcare institutions to repurpose areas not currently used to provide patient care into patient care spaces; when these patient care areas are no longer needed, they can be returned to their former state. PRN is an agile, integrated framework for healthcare environments that improves the quality of care and enhances the patient experience, no matter where health care is provided, by doing the following:
- Augmenting important real-time patient information into care processes
- Improving caregivers' efficiency by reducing or removing complicated interactions with technology
- Reducing patient-invasive touch without reducing care and personal interactions that increase satisfaction
- Engaging the patient and family in a way that reduces mental stress and improves satisfaction with care
- Allowing care to flex into alternate areas as needs arise and change (This Week Health, 2022, para. 2)
Therefore, PRN is making the processes, workflows, and technologies seamless.
Optimization
Most of what has been and will be discussed in this chapter is related to workflow analysis in conjunction with technology implementations. Nevertheless, not all workflow analysis and redesign occur before the implementation of technology. Some analysis and redesign efforts may occur weeks, months, or even years following the implementation. When workflow analysis occurs after implementation, it is often referred to as optimization. Optimization is the process of moving conditions past their current state and into more efficient and effective methods of performing tasks. Merriam-Webster (n.d.) defined optimization to be the act, process, or methodology of making something (as a design, system, or decision) as fully perfect, functional, or effective as possible. Some organizations will routinely engage in optimization efforts following an implementation, whereas other organizations may undertake this activity in response to clinicians' concerns or a marked change in operational performance.
Furthermore, workflow analysis can be conducted either as a stand-alone effort or as part of an operational improvement event. When the process is addressed alone, the effort is termed process improvement. Nursing informatics professionals should always be included in these activities to represent the needs of clinicians and to serve as a liaison for technological solutions to process problems. In addition, informaticists will likely become increasingly operationally focused and will need to transform their role accordingly to address workflow in an overall capacity as well as respective to technology. As mentioned earlier, hospitals tend to operate with smaller profit margins than other industries, and these profits will likely continue to diminish, forcing organizations to work smarter, not harder, and to use technology to accomplish this goal.
If optimization efforts are undertaken, the need to revisit workflow design should not be considered a flaw in the implementation approach. Even a well-designed future-state workflow during a technology implementation must be reexamined after implementation to ensure that what was projected about the future state remains valid and to incorporate any additional workflow elements into the process redesign.
Exploring the topic of workflow analysis regarding clinical technology implementation will yield considerably fewer literature results than searching for other topical areas of implementation. More research is needed in the area of the financial implications of workflow inefficiencies and their impact on patient care. Time studies require an investment of resources and may be subject to patient privacy issues as well as the challenges of capturing time measurements on processes that are not exactly replicable. Another confounding factor affecting the quality and quantity of workflow research is the lack of standardized terminology for this area. A comprehensive literature search was conducted and published through the AHRQ in 2008 as an evidence-based handbook for nurses; this literature search yielded findings indicating that a lack of standardized terminology in the area of workflow and publications on this topic have made it a difficult subject to support through research findings. Stitt (2021) outlined some of the difficulties associated with different operations and different terminologies found in IT operations and security operations. He described the two teams as typically opposing rather than cooperating for the good of the organization and stressed the need for them to speak a common language. “While things like terminology, user interface preferences and workflows will need to be addressed, getting alignment about the sources of data is an important first step, allowing decisions to be made based on a common set of information” (p. 11).
What all organizations ultimately strive for is efficient and effective delivery of patient care. The terms efficient and effective are widely known in quality areas, or Six Sigma and Lean departments, but are not necessarily known or used in informatics. Effective delivery of care or workflow suggests that the process or end product is in the most desirable state. An efficient delivery of care or workflow would mean that little waste-that is, unnecessary motion, transportation, overprocessing, or defects-was incurred. Some health systems, such as Virginia Mason University Village Medical Center, have experienced significant quality and cost gains from the widespread implementation of Lean throughout their organizations.
Workflow Analysis and Informatics Practice ⬆ ⬇
The American Nurses Association (ANA), in Nursing Informatics: Scope and Standards of Practice (2015, 2022), defined functional areas of practice for the informatics nurse specialist (INS). The functional area of analysis identified the specific functional qualities related to workflow analysis. Particularly, the ANA indicated that the INS should develop techniques necessary to assess and improve human-computer interaction. Workflow analysis is a central part of every INS function. The INS needs to understand workflow and appreciate how lack of efficient workflow negatively affects patient care.
A critical aspect of the informatics role is workflow design. Nursing informatics is uniquely positioned to engage in the analysis and redesign of processes and tasks surrounding the use of technology. The ANA (2015) cited workflow redesign as one of the fundamental skill sets that make up the discipline of this specialty. The ANA (2022) stated that the INS raises workflow and clinical practice awareness. Moreover, workflow analysis should be part of every technology implementation, and the role of the informaticist within this team is to direct others in the execution of this task or to perform the task directly.
Unfortunately, many nurses still find themselves in an informatics capacity without sufficient preparation for a process analysis role. One area of practice that is particularly susceptible to inadequate preparation is the ability to facilitate process analysis. Workflow analysis requires careful attention to detail and the ability to moderate group discussions, organize concepts, and generate solutions. These skills can be acquired through a formal academic informatics program or through courses that teach the concepts of Six Sigma or Lean by example. Regardless of where these skills are acquired, it is important to understand that they are now and will continue to be a vital aspect of the informatics role.
Some organizations have felt strongly enough about the need for workflow analysis that departments have been created to address this very need. Whether the department carries the name of clinical excellence, organizational effectiveness, or Lean Six Sigma, it is critical to recognize the value this group can offer technology implementations and clinicians.
As we examine how workflow analysis is conducted, note that although the nursing informaticist is an essential member of the team that participates in or enables workflow analysis, a team dedicated to this effort is necessary for its success.
Building the Redesign Team
The workflow redesign team is an interdisciplinary team consisting of process owners. Process owners are those persons who directly engage in the workflow to be analyzed and redesigned. These individuals can speak about the intricacy of the process, including process variations from the norm. When constructing the team, it is important to include individuals who are able to contribute information about the exact current state of the workflow and offer suggestions for improvement of its future state. Members of the workflow redesign team should also have the authority to make decisions about how the process should be redesigned. Sometimes this authority is issued by managers, or it could come from participation of the managers directly. Such a careful blend of decision-makers and process owners can be difficult to assemble but is critical for forming the team and enabling it to succeed. Often, individuals at the managerial level will want to participate exclusively in the redesign process. Although having management participate provides the advantage of having decision-makers and management-level buy-in, these individuals may also make erroneous assumptions about how the process should be versus how the process is truly occurring. Conversely, including only process owners who do not possess the authority to make decisions can slow down the work of the team while decisions are made outside the group sessions.
Team focus needs to be addressed at the outset of the team's assembly. Early on, the team should decide which workflow will be examined to avoid confusion or spending time unnecessarily on workflow that does not ultimately matter to the outcome. In the early stages of workflow redesign, the team should define the beginning and end and a few high-level steps of the process. Avoid focusing on process steps in great detail in the beginning because the conversation can get sidetracked or team members may get bogged down by focusing on details and not moving along at a good pace. Six Sigma expert George Eckes uses the phrase “Stay as high as you can as long as you can,” which is a great catchphrase to remember to keep the team focused and at a high level. The pace at which any implementation team progresses ultimately affects the overall timeline of a project; therefore, focus and speed are skills that the informatics expert should develop and use throughout every initiative but particularly when addressing workflow redesign.
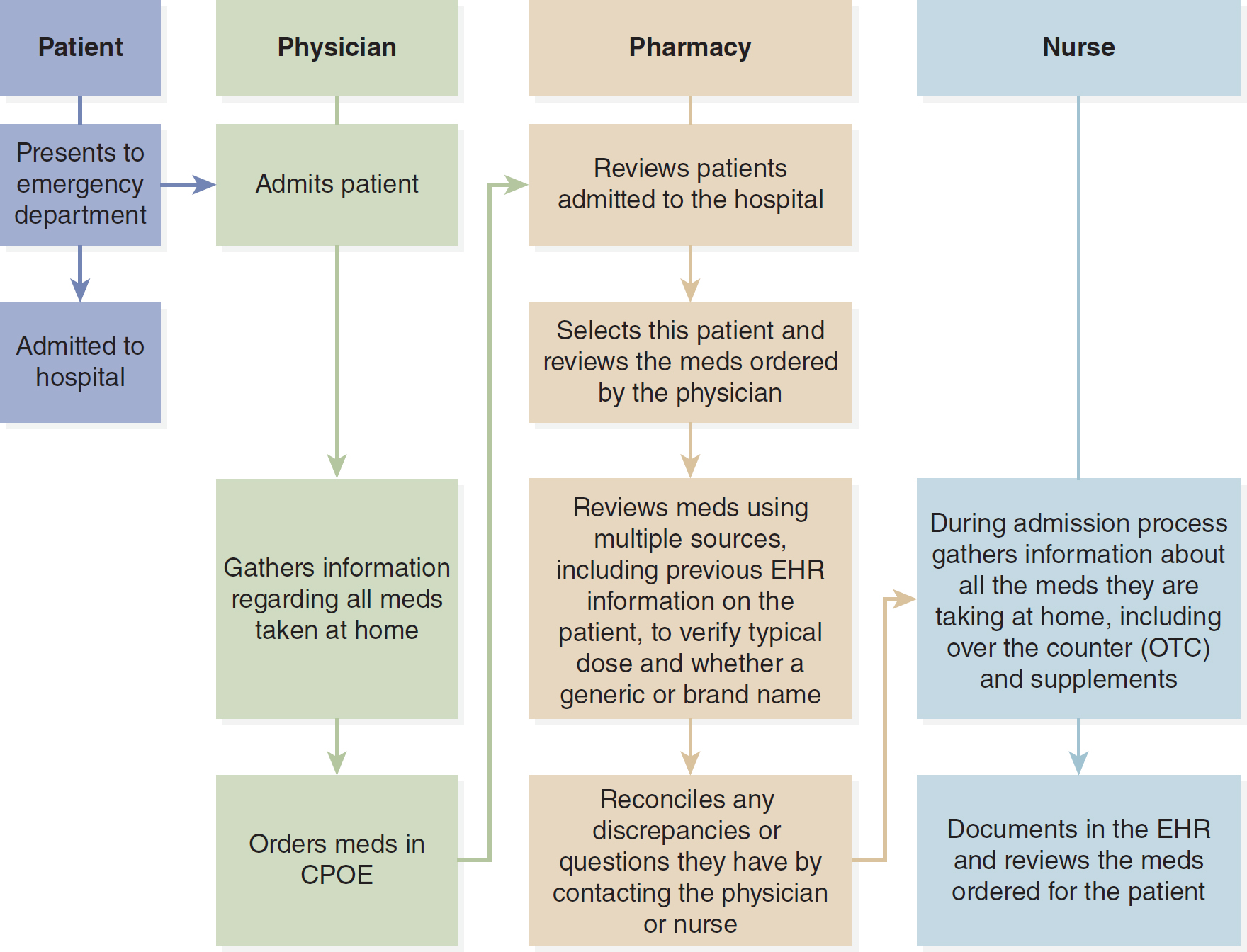
The workflow redesign team will develop a detailed process map after agreement is reached on the current state of the beginning and end points of the process and after a high-level map depicting the major process steps is finalized. Because workflow crosses many care providers, it may be useful to construct the process map using a swim-lane technique (Figure 13-2). A swim-lane technique uses categories, such as functional workgroups, and roles to visually depict groups of work and who performs the work. The resulting map shows how workflow and data transition to clinicians and can demonstrate areas of potential process and information breakdowns.
Figure 13-2 Swim-Lane Workflow: Process for Medication Reconciliation When a Patient Is Admitted to the Hospital
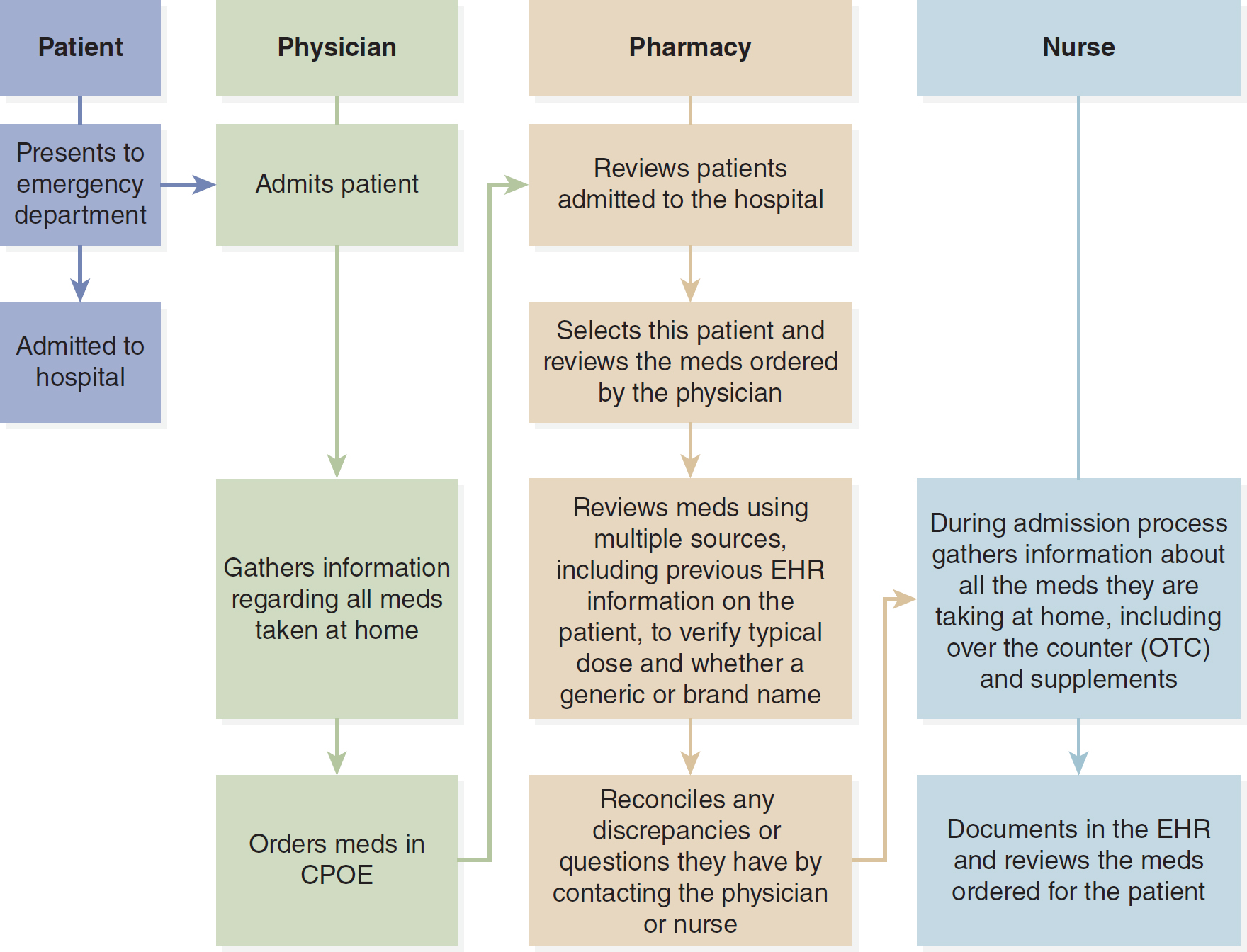
A flowchart outlines the process of reconciling medications when a patient is admitted to the hospital.
The diagram consists of four lanes representing Patient, Physician, Pharmacy, and Nurse. Steps include the following. 1. Patient: Presents to emergency department; Admitted to the hospital. 2. Physician: Admits the patient; Gathers information about all medications taken at home; Orders medications in C P O E. 3. Pharmacy: Reviews patients admitted to the hospital; Selects the patient and reviews medications ordered by the physician; Reviews medications using multiple sources, including previous E H R information on the patient, to verify typical dose and whether a generic or brand name; Reconciles any discrepancies or questions they have by contacting the physician or nurse. 4. Nurse: During admission process gathers information about all the medications they are taking at home, including over the counter, O T C, and supplements; Documents in the E H R and reviews medications ordered for the patient.
Developed by Dee McGonigle.
It may take several sessions of analysis to complete a process map as details are uncovered and workarounds discussed. There is a tendency for individuals who participate in process redesign sessions to describe workflow as they believe it to be occurring rather than how it really is. The informatics expert and/or the process team facilitator should determine what is really happening, however, and capture that information accurately. Regardless of whether a swim-lane or simplistic process map design is used, the goal is to capture enough details to accurately portray the process as it is happening today.
Besides process mapping, other techniques may be used to help the team understand the workflow as it exists in its current state. Future-state workflow planning will only be as good as the reliability of the current state; thus, it is crucial to undertake whatever other actions are needed to better understand what is happening in the current state. Observation, interviews, and process or waste walks are also helpful in understanding the current state. Waste walks are a method of observing work as it is performed to note any waste or inefficient practices. It is important to make sure that all findings are shared with the nurses who were observed.
Value Added Versus Non-Value Added
Beyond analysis of tasks, current-state mapping provides the opportunity for the process redesign team to distinguish between value-added and non-value-added activities. A value-added step is one that ultimately brings the process closer to completion or changes the product or service for the better. An example of a value-added step would be placing a name tag on a specimen sample. The name tag is necessary for the laboratory personnel to identify the specimen, and therefore its placement is an essential, or value-added, step in the process. Some steps in a process do not necessarily add value but are needed for regulatory or compliance reasons; therefore, they must be included in the future process. In contrast, a non-value-added step does not alter the outcome of a process or product. Activities such as handling, moving, and holding are not considered value-added steps and should be evaluated during workflow analysis. Manipulating papers, moving through computer screens, and walking or transporting items are considered non-value-added activities.
The five whys represent one technique for driving the team toward identifying value-added versus non-value-added steps. The process redesign facilitator will query the group about why a specific task is done or is done in a particular way through a series of questions asking why. The goal is to uncover tasks that came about due to workarounds or for other unsubstantiated reasons. Tasks that are considered non-value added and that are not necessary for the purpose of compliance or regulatory reasons should be eliminated from the future-state process. The team's purpose in redesigning workflow is to eliminate steps in a process that do not add value to the end state or that create waste by their very nature.
Waste
A key underpinning of the Lean philosophy is the removal of waste activities from workflow. Waste is classified as unnecessary activities or an excess of products used to perform tasks. The seven categories listed here are the most widely recognized forms of waste:
- Overproduction: pace is faster than necessary to support the process
- Waiting
- Transport
- Inappropriate processing: overprocessing
- Unnecessary inventory: excess stock
- Unnecessary motion: bending, lifting, moving, and so on
- Defects: reproduction
Variation
The nature of the work situation for the nurse is one of frequent interruptions, which cause the workflow to be disrupted and increase the chance of error (Wang & Jin, 2021; Yuan et al., 2013). Variation in workflow is considered the enemy of all good processes and therefore should be eliminated when possible. Variation occurs when workers perform the same function in different ways. This situation usually arises because of flaws in the way a process was originally designed, lack of knowledge about the process, or inability to execute a process as originally designed due to disruption or disturbances in the workflow. Examining the process as it exists today will help with identifying variation. Some variation cannot be eliminated because processes that involve highly customized products or services are generally not conducive to standardization and the elimination of variation inherent to the process.
Some people argue that delivery of care is subject to variation owing to its very nature and to the individual needs of patients. There is little doubt that each patient's care should be tailored to meet their specific needs. Nevertheless, delivery of care involves some common processes that can be standardized and improved upon without jeopardizing care.
Transitioning to the Future State
Following redesign efforts, regardless of whether they occurred during or after an implementation or as a stand-alone process improvement event, steps must be taken to ensure that change takes hold and that the new workflow continues after the support team has disbanded. Management support and involvement during the transition phase is essential because management will be necessary to enforce new workflow procedures and further define and refine roles and responsibilities. Documentation of the future-state workflow should have occurred during the redesign effort but is not completely finished until after the redesign is complete and the workflow has become operational. Policies and procedures are addressed and rewritten to encompass the changes to workflows and role assignments. Help desk, system analyst, nursing education, and other support personnel need to be educated about the workflow specifics as part of the post-improvement effort. It is considered good practice to involve the operational staff in the future process discussions and planning in order to incorporate specifics of these areas and to ensure staff buy-in.
Workflow changes beginning to fail and workarounds developing signal that something is flawed about the way in which the new process was constructed and that it needs to be evaluated further. The workflow redesign team is then brought together to review and, if necessary, redesign the process.
The future state is constructed with the best possible knowledge of how the process will ideally work. To move from the current state to the future state, gap analysis is necessary. Gap analysis zeroes in on the major areas most affected by the change-namely, technology. What often happens in redesign efforts is an exact or near-exact replication of the current state using automation. The gap analysis discussion should generate ideas from the group about how best to utilize the technology to transform practice. A prudent step is to consider having legal and risk representatives at the table when initiating future-state discussions to identify the parameters within which the group should work; nevertheless, the group should not assume that the existing parameters are its only boundaries.
Future-state process maps become the basis of educational materials for end users, communication tools for the project team, and the foundation of new policies and procedures. Simplified process maps provide an excellent schematic for communicating change to others.
Informatics as a Change Agent ⬆ ⬇
Technology implementations represent a significant change for clinicians, as does the workflow redesign that accompanies adoption of technology. Often, the degree of change and its impact are underappreciated and unaccounted for by leadership and staff alike. A typical response to change is anger, frustration, and a refusal to accept the proposed change. All these responses should be expected and need to be accounted for; thus, a plan to address the emotional side of change is developed early on. Every workflow redesign effort should begin with a change management plan (Figure 13-3). Engagement of the end user is a critical aspect of change management and therefore technology adoption. Without end user involvement, change is resisted and efforts are subject to failure. Users may be engaged and brought into the prospective change through question-and-answer forums, technology demonstrations, and frequent communications regarding change and as department-specific representatives in working meetings.
Figure 13-3 Change Management

A graphic reads Change.
© Digital Storm/Shutterstock
Many change theories have been developed. No matter which change theory is adopted by the informatics specialist, however, communication, planning, and support are key factors in any change management strategy. Informaticists should become knowledgeable about at least one change theory and use this knowledge as the basis for change management planning as part of every effort. John Kotter (1996), one of the most widely recognized change theorists, suggested that the following conditions must be addressed to deal with change in an organization:
- Education and communication
- Participation and involvement
- Facilitation and support
- Negotiation and agreement
- Manipulation and cooptation
- Explicit and implicit coercion
In the Healthcare Information and Management Systems Society (HIMSS) (2022) Nursing Informatics Workforce Survey, the crucial role that nurse informaticists play in enhancing healthcare, driving innovation and technology to achieve the full health promise of every human, was validated. Nurse informaticists “use project and change management expertise and optimize electronic medical health records, quality initiatives and reporting” (HIMSS, 2022, para. 1). Nursing informaticists are the most significant resource in a project team that influences adoption and change management since they bring to such teams their ability to interact with various clinicians, knowledge of clinical practice, and the ability to empathize with the clinicians as they experience the impact of workflow change. These innate skills differentiate the nursing informaticist from other members of the implementation team and are highly desirable in the informatics community.
Nevertheless, no matter which change management techniques are employed by the informatics specialist and the project team, the adoption of technology and workflow may be slow to evolve. Change is often a slow process that requires continual positive reinforcement and involvement of supporting resources. Failure to achieve strong adoption results early on is not necessarily a failure of the methods utilized but rather may be due to other factors not entirely within the control of the informaticist.
Perhaps a complete alteration in behavior is not possible, but modifications to behaviors needed to support a desired outcome can be realized. This situation is analogous to the individual who stops smoking; the desire for the cigarette remains, but the behavior has been modified to no longer sustain smoking. To manage change in an organization, nurses must modify behavior to produce the intended outcome.
Change takes hold when strong leadership support exists. This support manifests itself as a visible presence to staff, clear and concise communications, an unwavering position, and an open-door policy to field concerns about change. Too often, leadership verbally endorses change and then fails to follow through with these actions or withdraws support when the going gets tough. Inevitably, if leadership wavers, so, too, will staff.
Measuring the Results ⬆ ⬇
Metrics provide an understanding about the performance of a process or function. Typically, within clinical technology projects, metrics about the performance of the technology or that capture the level of participation or adoption are identified and collected. Equally important is the need for process performance metrics. Process metrics are collected at the initial stage of project or problem identification. Current-state metrics are then benchmarked against internal indicators. When there are no internal indicators to benchmark against, a suitable course of action is to benchmark against an external source, such as a similar business practice within a different industry. Consider examining the hotel room changeover strategy or the customer service approach of Disney or Ritz-Carlton hotels, for example, to determine suitable metrics for a particular project or focus area.
The right workflow complement will provide the organization with the data it needs to understand operational and clinical performance. This area is highlighted through the need for healthcare organizations to capture MACRA measures. Good metrics should tell the story of accomplishment. The presence of technology alone does not guarantee an organization's ability to capture and report on these measures without also addressing the surrounding workflow. Metrics should focus on the variables of time, quality, and costs. Table 13-1 provides examples of relevant metrics.
Table 13-1 Examples of MetricsTurnaround times | Cycle times | Throughput |
|---|
Changeover time | Setup time | System availability |
Patient satisfaction | Employee satisfaction | |
MACRA highlights the need for healthcare organizations to collect information that represents the impact of technology on patient outcomes. Furthermore, data are necessary to demonstrate how a process is performing in its current state. In spite of the MACRA mandates, the need to collect data to demonstrate improvement in workflow-though it remains strong-is all too often absent in implementation or redesign efforts. A team cannot demonstrate improvements to an existing process without collecting information about how the process is performing today. Current-state measures also help the process team validate that the correct area for improvement was identified. Once a process improvement effort is over and the new solution has been implemented, post-improvement measures should be gathered to demonstrate progress.
In some organizations, the informatics professional reports to the director of operations, the chief information officer, or the chief operations officer. In this relationship, the need to demonstrate operational measures is even stronger. Some of the operational measures captured are turnaround times, throughput, and equipment or technology availability.
Quality Improvement Initiatives ⬆ ⬇
Thus far, we have focused on workflow considerations in relation to the adoption, implementation, and optimization of new technology. We turn now to another critical role for the nurse informaticist, quality improvement (QI). QI consists of a systematic process using data and continuous actions that leads to measurable improvement in healthcare services and the health status of targeted patient groups. QI projects use many of the same techniques that we discussed for workflow-namely, process mapping, team buy-in, and attention to change theories. They are also dependent on metrics to accurately assess the nature of the issue to be addressed and to measure the success of the project. Health Catalyst (2022) suggested the following broad categories for potential hospital QI projects: “clinical variation, preventable medical errors, hospital acquired infections, delays in patient discharge, and dwindling cash flow” (para. 1). As with any project, it is critical to choose wisely; select the topic to address, a great team, a process that is likely to succeed, and the most reliable metrics. In addition to relational skills, such as collaboration and communication, Jones et al. (2019) identified these key characteristics that QI change agents need: “[e]nthusiasm, optimism, curiosity, and perseverance” (para. 5).
Systematic change requires attention to the processes and metrics necessary to successfully enact the change. QI is dependent on four key principles for success: the need to understand current systems and processes, to focus on patient needs and expectations, to focus on teamwork, and to be data driven. The Somerset NHS Foundation Trust (n.d.) outlined the following seven key steps in a QI project:
- Select the QI team members based on their knowledge of the issue to be solved and their ability to contribute meaningfully to the team.
- Select the project by considering performance gaps, the problem, the relationship to the organization's strategic plan, staff input and/or resistance, and feasibility and timing.
- Develop the aim statement using a SMART (specific, measurable, achievable, relevant, and time-bound) approach. The aim statement should be specific enough so that the what, why, who, when, and how of the project are readily apparent.
- Develop measures to determine whether project goals were met while keeping in mind that a change in one area may create issues for another area. A QI project must consider these critical organizational balancing issues.
- Identify change ideas.
- Test changes.
- Develop a process for sustainability and spread.
You should always celebrate success. This is a necessary component and time well spent, but it does not always occur. Reflecting on and appreciating the work that went into the project and celebrating its success are critical to recognizing this effort and the desired outcomes.
Future Directions ⬆ ⬇
Workflow analysis is not an optional part of clinical implementations but rather is a necessity for safe patient care supported by technology. The ultimate goal of workflow analysis is to create a future-state solution that maximizes the use of technology and eliminates non-value-added activities. Although many tools are available to accomplish workflow redesign, the best method is the one that complements the organization and supports the work of clinicians. Redesigning how people do work will provide evidence to create change; thus, the nursing informaticist will need to apply change management principles for the new way of doing things to take hold. These statements are also true of QI projects.
Workflow analysis and QI have been described in this chapter within the context of the most widely accepted tools that are fundamentally linked to the concepts of Lean Six Sigma. Other methods of workflow analysis and QI exist and may also be used to assess clinical workflow. An example of an alternative workflow analysis tool is the use of radio-frequency badges to detect movement within a defined clinical area. Clinician and patient movements may be tracked using these devices, and corresponding actions may be documented, which together paint a picture of the workflow for a specific area (Vankipuram et al., 2011).
Another example of a workflow analysis tool involves the use of modeling software. An application such as ProModel provides images of the clinical work area where clinician workflows can be plotted out and reconfigured to best suit the needs of a specific area. Simulation applications enable decision-makers to visualize realistic scenarios and draw conclusions about how to leverage resources, implement technology, and improve performance. Other vendors that offer simulation applications include Maya and Autodesk.
Healthcare organizations need to consider how other industries have analyzed and addressed workflow to streamline business practices and improve quality outputs to glean best practices that might be incorporated into the healthcare industry's own clinical and business approaches. First, however, each healthcare organization must step outside itself and recognize that not all aspects of patient care are unique; consequently, many aspects of care can be subjected to standardization. Many models of workflow redesign from manufacturing and the service sector can be extrapolated to health care. The healthcare industry is facing difficult economic times and can benefit from performance improvement strategies used in other industries.
Although workflow analysis principles have been described in this chapter within the context of acute and ambulatory care, the need to perform process analysis on a macro level will expand as more organizations move forward with health information exchanges (HIEs) and medical home models. An HIE requires the nursing informaticist to visualize how patients move through the entire continuum of care and not just a specific patient care area.
Technology initiatives will become increasingly complex in the future. In turn, nursing informaticists will need greater preparation in the area of process analysis and improvement techniques to meet the growing challenges that technology brings and the operational performance demands of fiscally impaired healthcare organizations.
Summary ⬆ ⬇
Workflows integrating technology provide the healthcare professional with the data necessary to make informed decisions. This quality data must be collected and captured to meet MACRA measures. Nurses are the healthcare team members who spend the most time with patients. Therefore, the nurses must be involved in “meaningful data collection and reporting. Documentation by nurses can tell what's going on with the patient beyond physical exams, test results, and procedures” (Daley, 2011, para. 5).
Workflow redesign is a critical aspect of technology implementation. When done well, it yields technology that is more likely to achieve the intended patient outcomes and safety benefits. Nursing informatics professionals are taking on a greater role regarding workflow design, and this aspect of practice will grow in light of MACRA-driven measures. QI initiatives that affect hospital performance will also drive informatics professionals to influence how technology is used in the context of workflow and QI to improve the bottom line for their organizations. In an ideal world, nurse informaticists who are experts at workflow analysis and QI would be core members of every organization.
| Thought-Provoking Questions |
|---|
- What do you perceive as the current obstacles to redesigning workflow within your clinical setting?
- Thinking about your last implementation, were you able to challenge the policies and practices that constitute today's workflow, or were you able to create a workflow solution that eliminated non-value-added steps?
- Is the workflow surrounding technology usage providing the healthcare organization with the data it needs to make decisions and eventually meet MACRA criteria?
- Describe your understanding of the PRN in detail. How is the PRN disrupting healthcare delivery?
- How does the current educational preparation need to change to address the skills necessary to perform workflow analysis and QI?
- Identify a process that would benefit from a QI project. Whom would you place on the team, and what steps would you initiate?
|
References ⬆
- Abraham J., Kannampallil T. G., Jarman A., Sharma S., Rash C., Schiff G., & Galanter W. (2018). Reasons for computerised provider order entry (CPOE)-based inpatient medication ordering errors: An observational study of voided orders. BMJ Quality & Safety, 27(4), 299-307. http://dx.doi.org/10.1136/bmjqs-2017-006606
- Agency for Healthcare Research and Quality. (n.d.). Workflow assessment for health IT toolkit. https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit
- Agency for Healthcare Research and Quality. (2008). Patient safety and quality: An evidence-based handbook for nurses. https://archive.ahrq.gov/professionals/clinicians-providers/resources/nursing/resources/nurseshdbk/nurseshdbk.pdf
- American Nurses Association. (2015). Nursing informatics: Scope and standards of practice (2nd ed.). Nursesbooks.org
- American Nurses Association. (2022). Nursing informatics: Scope and standards of practice (3rd ed.). Nursesbooks.org
- American Society for Health Care Risk Management. (2021). ASHRM patient safety tip sheet: Technology and patient safety. www.ashrm.org/system/files/media/file/2021/02/Technology-and-Patient-Safety.pdf
- Ash J. S., Sittig D. F., Dykstra R., Campbell E., & Guappone K. (2009). The unintended consequences of computerized provider order entry: Findings from a mixed methods exploration. International Journal of Medical Informatics, 78(Suppl 1), S69-S76. http://dx.doi.org/10.1016/j.ijmedinf.2008.07.015
- Bucur A., van Leeuwen J., Christodoulou N., Sigdel K., Argyri K., Koumakis L., Graf N., & Stamatakos G. (2016). Workflow-driven clinical decision support for personalized oncology. BMC Medical Informatics & Decision Making, 16(Suppl 2), 151-162. http://dx.doi.org/10.1186/s12911-016-0314-3
- Campbell E., Guappone K., Sittig D., Dykstra R., & Ash J. (2009). Computerized provider order entry adoption: Implications for clinical workflow. Journal of General Internal Medicine, 24(1), 21-26. https://doi.org/10.1007/s11606-008-0857-9
- Centers for Medicare and Medicaid Services. (2016a). CMS quality measure development plan: Supporting the transition to the Merit-based Incentive Payment System (MIPS) and Alternative Payment Models (APMs). www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/Final-MDP.pdf
- Centers for Medicare and Medicaid Services. (2016b). Quality Payment Program: APMs overview. https://qpp.cms.gov/apms/overview
- Centers for Medicare and Medicaid Services. (2021). 2018 program requirements Medicare.www.cms.gov/medicare/regulations-guidance/promoting-interoperability-programs/requirements-previous-years/2018-program-requirements-medicare
- Centers for Medicare and Medicaid Services. (2022). Requirements for previous years. www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/RequirementsforPreviousYears.html
- Cision PR Newswire. (2018, May 10). Nursing EHR satisfaction takes a major swing to the positive, Black Book user survey. www.prnewswire.com/news-releases/nursing-ehr-satisfaction-takes-a-major-swing-to-the-positive-black-book-user-survey-300646654.html
- Clancy T., Delaney C., Morrison B., & Gunn J. (2006). The benefits of standardized nursing languages in complex adaptive systems such as hospitals. Journal of Nursing Administration, 36(9), 426-434. http://dx.doi.org/10.1097/00005110-200609000-00009
- Daley K. (2011). Making HIT meaningful for nursing and patients. American Nurse, 43(4), 3. www.ncbi.nlm.nih.gov/pubmed/21954800
- Earl M., Sampler J., & Short J. (1995). Strategies for business process reengineering: Evidence from field studies. Journal of Management Information Systems, 12(1), 31-56. https://doi.org/10.1080/07421222.1995.11518069
- Flohr L., Beaudry S., Johnson K. T., West N., Burns C. M., Ansermino J. M., Dumont G. A., Wensley D., Skippen P., & Gorges M. (2018). Clinician-driven design of VitalPAD-An intelligent monitoring and communication device to improve patient safety in the intensive care unit. IEEE Journal of Translational Engineering in Health and Medicine, 6, 1-14. http://dx.doi.org/10.1109/JTEHM.2018.2812162
- Gugerty B., Maranda M. J., Beachley M., Navarro V. B., Newbold S., Hawk W., Karp J., Koszalka M., Morrison S., Poe S. S., & Wilhelm D. (2007). Challenges and opportunities in documentation of the nursing care of patients. Maryland Nursing Workforce Commission. http://mbon.maryland.gov/Documents/documentation_challenges.pdf
- Healthcare Information and Management Systems Society. (2022). HIMSS Nursing Informatics Workforce Survey.www.himss.org/resources/himss-nursing-informatics-workforce-survey
- Health Catalyst. (2021, January 21). Healthcare process improvement: Six strategies for organizationwide transformation.www.healthcatalyst.com/insights/healthcare-process-improvement-6-strategies
- Health Catalyst. (2022, July 5). The top four examples of quality improvement in healthcare. www.healthcatalyst.com/insights/top-examples-quality-improvement-healthcare
- Holston F. (2022, August 2). What is Patient Room ‘Next' and how can healthcare organizations achieve it? HealthTech. https://healthtechmagazine.net/article/2022/08/what-patient-room-next-and-how-can-healthcare-organizations-achieve-it
- Hopkins B. (2019, August 23). 3 ways to improve healthcare workflow. Medical Group Management Association. www.mgma.com/articles/3-ways-to-improve-healthcare-workflow
- Jones B., Vaux E., & Olsson-Brown A. (2019). How to get started in quality improvement. British Medical Journal, 364, k5408. https://doi.org/10.1136/bmj.k5437
- Kotter J. P. (1996). Leading change. Harvard Business School Press.
- Laoyan S. (2023). 7 types of process improvement methodologies. Asana.
- Merriam-Webster. (n.d.). Optimization. In Merriam-Webster.com dictionary. Retrieved July 17, 2023, from www.merriam-webster.com/dictionary/optimization
- Schoenbaum A., & Carroll W. (2021). Nursing informatics key role in defining clinical workflow, increasing efficiency and improving quality. Healthcare Information and Management Systems Society. www.himss.org/resources/nursing-informatics-key-role-defining-clinical-workflow-increasing-efficiency-and
- Somerset NHS Foundation Trust. (n.d.). 7 steps to quality improvement. https://web.archive.org/web/20230206123730/https://www.somersetft.nhs.uk/improvement/improvement/7-steps-to-qi
- Stitt T. (2021). Office walls and roadblocks: How workflows and terminology get in the way of visibility. Network Security, 2019(11), 9-13. https://doi.org/10.1016/S1353-4858(19)30131-X
- Stokowski L. (2013, September 12). Electronic nursing documentation: Charting new territory. Medscape. www.medscape.com/viewarticle/810573_1
- The Patient Safety League. (2023). You're not immune to medical errors.4patientsafety.org
- This Week Health. (2022, September 8). Future of care: Patient Room ‘Next' with Sirius Healthcare.https://thisweekhealth.com/futureofcare-prn-sirius-healthcare
- Thompson C., Kell C., Shetty R., & Banerjee D. (2016). Clinical workflow redesign leveraging informatics improves patient outcomes. Heart & Lung, 45(4), 380-381. https://doi.org/10.1016/j.hrtlng.2016.05.025
- Vankipuram M., Kaholab K., Cohenac T., & Patel V. L. (2011). Toward automated workflow analysis and visualization in clinical environments. Journal of Biomedical Informatics, 44(3), 432-440. https://doi.org/10.1016/j.jbi.2010.05.015
- Wang W., & Jin L. (2021). Current status and influencing factors of nursing interruption events. American Journal of Managed Care, 27(6). www.ajmc.com/view/current-status-and-influencing-factors-of-nursing-interruption-events
- Yuan M., Finley G., Long J., Mills C., & Johnson R. (2013). Evaluation of user interface and workflow design of a bedside nursing clinical decision support system. Interactive Journal of Medical Research, 2(1), e4. https://doi.org/10.2196/ijmr.2402