Objectives ⬇
- Provide an overview of community and population health informatics.
- Assess informatics tools for promoting community and population health.
- Explore the roles of federal, state, and local public health agencies in the development of public health informatics.
Key Terms ⬆ ⬇
Introduction ⬆ ⬇
The need for informatics tools to promote and support public health has never been more apparent. Note the following global public health crises of the past two decades alone: SARS, MERS, Ebola, H1N1 (swine flu), Zika, and COVID-19.
In the late fall of 2002, severe acute respiratory syndrome (SARS), the first of several novel coronaviruses, appeared in China. By March 2003, SARS had become recognized as a global threat. According to data from the World Health Organization (WHO; 2021), more than 8,000 people from 29 countries became infected with this previously unknown virus, and more than 700 people died. By 2004, the last SARS cases were caused by laboratory-acquired infections. Because of computerized global data collection, the potentially negative effect of a widespread global epidemic was averted. Middle East respiratory syndrome (MERS) emerged in Saudi Arabia in 2012 and was primarily limited to Arabian countries, with a mortality rate of 3 or 4 out of 10 cases (Centers for Disease Control and Prevention [CDC], 2015). In the late fall of 2019, SARS-CoV-2 (COVID-19) emerged in Wuhan, China; spread rapidly around the world; and was declared a pandemic by the WHO on March 11, 2020 (Felman, 2021). This pandemic resulted in lockdowns in many countries with policies for extreme social distancing enforced to slow the spread of the disease.
Previous pandemic declarations had all been related to flu viruses: H1N1 in 1918, H2N2 from 1957 to 1958, H3N2 in 1968, and H1N1 in 2009 (CDC, 2018b). The 2009 H1N1 swine flu outbreak infected 60.8 million people in the United States, with a mortality rate of 0.2% (Hickok, 2020). Klobucista and Renwick (2020) reported that during the 2014 Ebola epidemic, 11,316 people died, with most cases confined to West Africa. As the Zika virus threat emerged, the CDC (2022d) reported that its Emergency Operations Center (EOC)
was activated for Zika on January 22, 2016, and moved to a level 1 activation-the highest level-on February 8, 2016. The EOC is the command center for monitoring and coordinating the emergency response to Zika, bringing together CDC scientists with expertise in arboviruses like Zika, reproductive health, birth defects and developmental disabilities, and travel health. (para. 1)
The CDC's EOC staff works in collaboration with local, national, and international response partners to analyze, validate, and efficiently exchange information about outbreaks.
As nurses navigated these outbreaks, they appreciated the need for timely information to be shared with the world population as well as with the healthcare workers responsible for caring for them. Modjarrad et al. (2016) reported on a WHO meeting in which participants “recognized that it is not enough for parties to simply agree, in principle, on sharing primary data, as the world must also commit to tackling the technical challenges of implementing data sharing agreements by simplifying and standardizing data capture procedures, assuring data quality, and harmonizing disparate data platforms” (para. 5). These concepts are central to informatics.
The CDC (2022c) public health surveillance center defines surveillance as “the collection, analysis and use of data to target public health prevention. It is the foundation of public health practice” (para. 1). The CDC provides interactive databases and surveys, as well as methods, to guide conducting and evaluating surveillance systems and data standardization. In 2018, Lee et al. reported that the CDC had more than 110 surveillance systems, many of them for single diseases or conditions that were added as a need arose, which resulted in poor coordination and burdensome experiences for users.
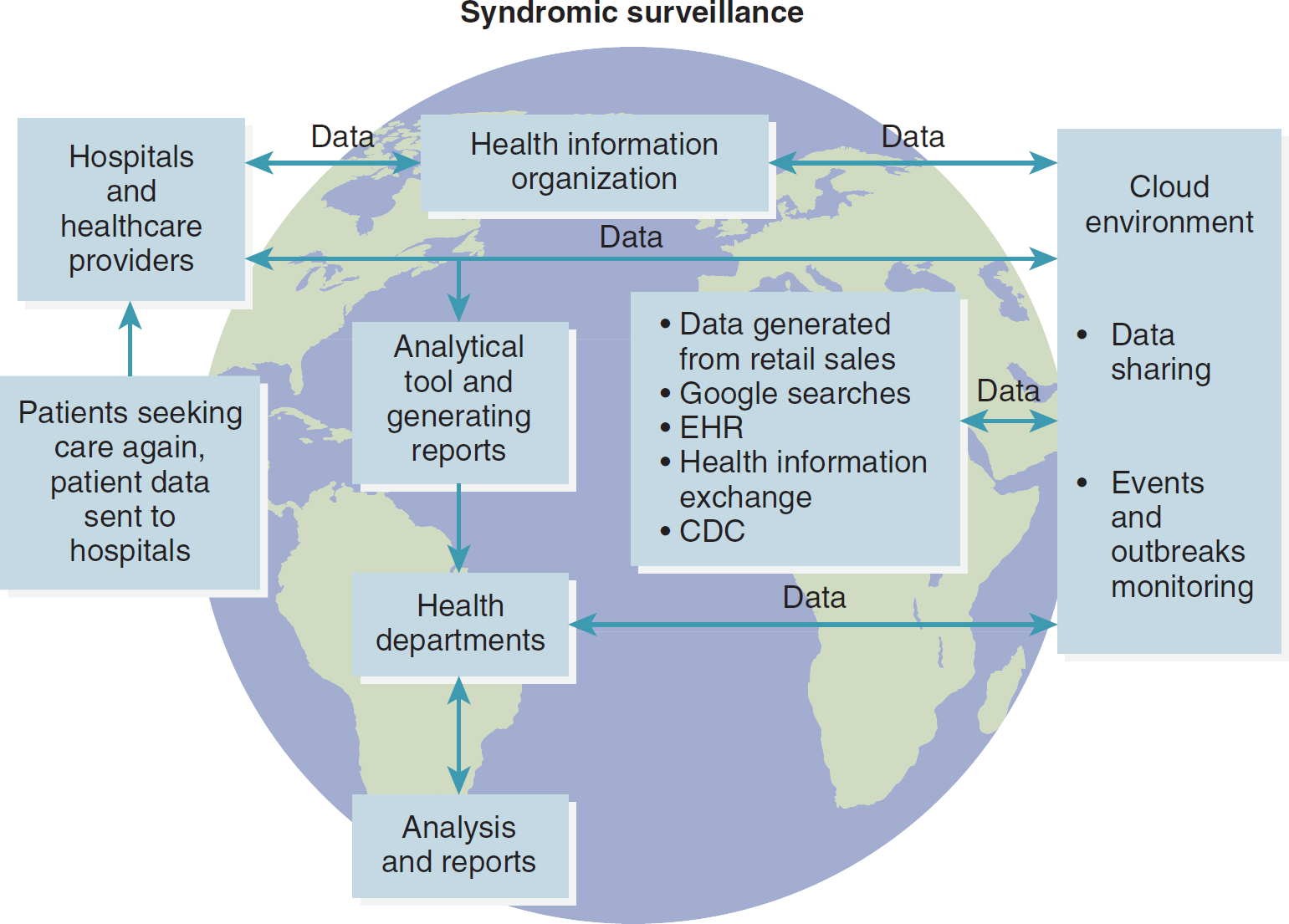
Many surveillance systems, loosely termed syndromic surveillance systems, use data that are not diagnostic of a disease but that might indicate the early stages of an outbreak (see Figure 17-1). Outbreak detection is the overriding purpose of syndromic surveillance for terrorism preparedness. Enhanced case finding and monitoring the course and population characteristics of a recognized outbreak are also potential benefits of syndromic surveillance. In recent years, new data have been used by public health officials to enhance surveillance, such as patients' chief complaints in emergency departments, ambulance log sheets, prescriptions filled, retail drug and product purchases, school or work absenteeism, and medical signs and symptoms in persons seen in various clinical settings. With faster, more specific, and more affordable diagnostic methods and decision support tools, timely recognition of reportable diseases with the potential to lead to a substantial outbreak is now possible. Tools for pattern recognition can be used to screen data for patterns needing further public health investigation. For example, during the 2003 SARS epidemic, the Centers for Disease Control and Prevention (CDC) worked to develop surveillance criteria to identify persons with SARS in the United States, and the surveillance case definition changed throughout the epidemic to reflect increased understanding of SARS (CDC, 2017). At this writing, COVID-19 surveillance is ongoing and consists of several data sources, including but not limited to virus and flu surveillance systems, academic systems, case reporting systems, research labs, and commercial testing labs. The CDC (2023b) lists the following goals for COVID-19 surveillance:
Figure 17-1 Syndromic Surveillance System
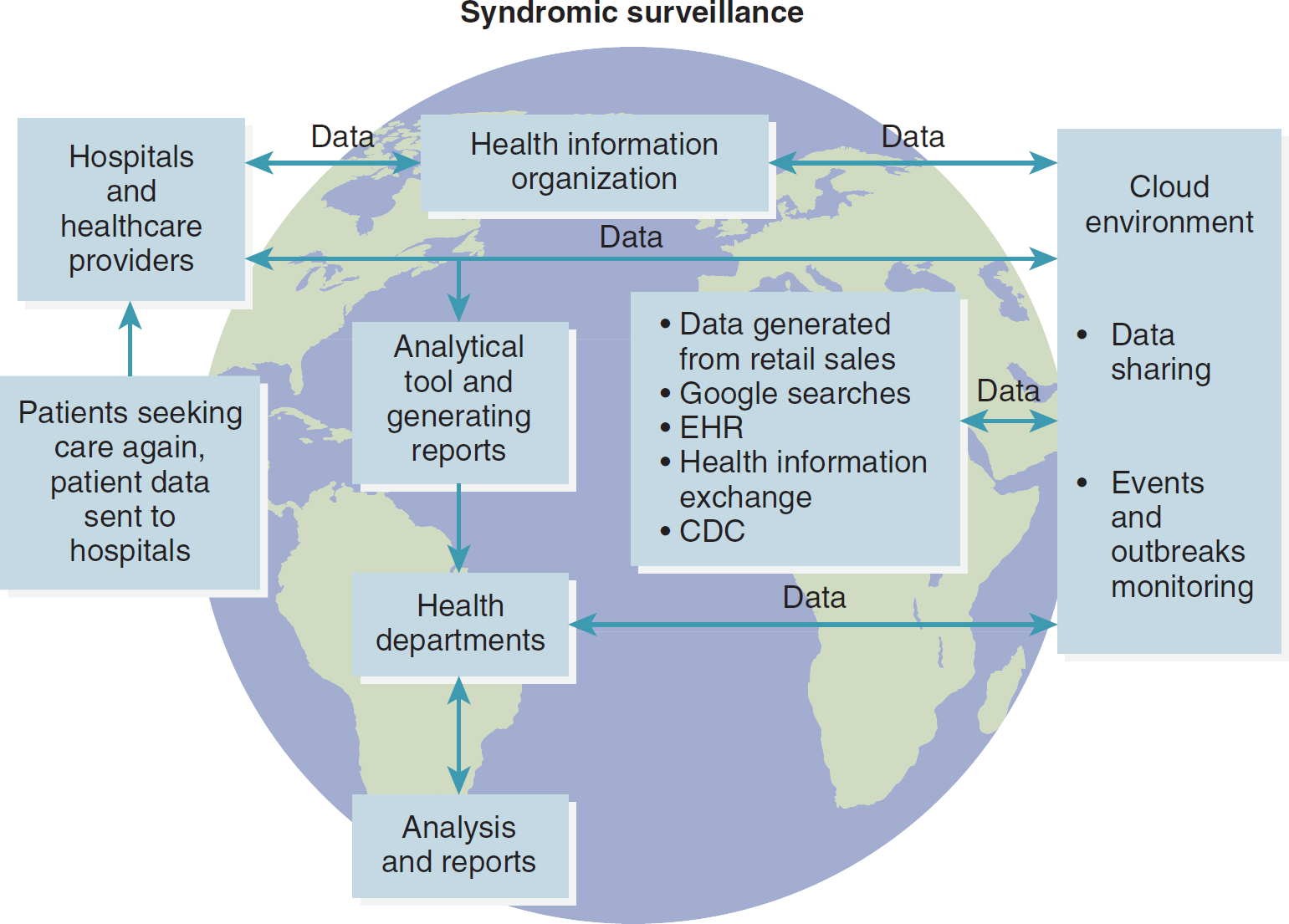
A flowchart overlaid on a globe depicts the process of syndromic surveillance.
The process begins with patients seeking care, their data sent to hospitals and healthcare providers. From there, it reaches a Health Information Organization, continuing through data to a Cloud environment involving data sharing and events and outbreaks monitoring. The Cloud environment, through data generated from various sources like retail sales, Google searches, E H R, Health Information Exchange, and C D C, leads to analytical tools and report generation. The final stages involve the dissemination of reports to Health Departments for analysis and reporting.
- To monitor spread and intensity of COVID-19 disease in the United States
- To understand disease severity and the spectrum of illness
- To understand risk factors for severe disease and transmission
- To monitor for changes in the virus that causes COVID-19
- To estimate disease burden
- To produce data for forecasting COVID-19 spread and impact (para. 3)
Information acquired by the collection and processing of population health data becomes the basis for knowledge in the field of public health. There is an ever-increasing need for timely information about the health of communities, states, and countries. Knowledge about disease trends and other threats to community health can improve program planning, decision-making, and care delivery. Patients seen from the perspective of major health threats within their communities can benefit from opportunities for early intervention.
This chapter focuses on the application of informatics methods to public health surveillance. The availability of clinical information for public health has been fundamentally changed by the introduction of the electronic health record (EHR) and health information technology (IT), both of which allow for the efficient collection and sharing of data that can be “leveraged for quality improvement and prevention activities” (HealthIT.gov, 2023a, para. 1).
Public Health Essential Services ⬆ ⬇
Public health focuses on health promotion and disease prevention. According to the CDC Foundation (n.d.),
[p]ublic health is the science of protecting and improving the health of people and their communities. This work is achieved by promoting healthy lifestyles, researching disease and injury prevention, and detecting, preventing and responding to infectious diseases.
Overall, public health is concerned with protecting the health of entire populations. These populations can be as small as a local neighborhood, or as big as an entire country or region of the world. (para. 1-2)
In the late 1980s the core public health functions were identified as assessment, policy development, and assurance. However, these categories were so broad that they did not provide direction for public health practitioners. In the 1990s, a task force identified 10 essential services of public health, which better defined how local health departments could protect community health (Correll, 2022).
The essential functions as defined by the CDC (2023c) are as follows:
- Assess and monitor population health status, factors that influence health, and community needs and assets
- Investigate, diagnose, and address health problems and hazards affecting the population
- Communicate effectively to inform and educate people about health, factors that influence it, and how to improve it
- Strengthen, support, and mobilize communities and partnerships to improve health
- Create, champion, and implement policies, plans, and laws that impact health
- Utilize legal and regulatory actions designed to improve and protect the public's health
- Assure an effective system that enables equitable access to the individual services and care needed to be healthy
- Build and support a diverse and skilled public health workforce
- Improve and innovate public health functions through ongoing evaluation, research, and continuous quality improvement
- Build and maintain a strong organizational infrastructure for public health (para. 3)
What Is Public Health Informatics? ⬆ ⬇
Historically, Dr. John Snow can be designated as the “father” of public health informatics (PHI) (Figure 17-2). In 1854, he plotted information about cholera deaths and was able to determine that the deaths were clustered around the same water pump in London. He convinced authorities that the cholera deaths were associated with that water pump; when the pump handle was removed, the cholera outbreak ended. It was Dr. Snow's focus on the cholera-affected population as a whole rather than on a single patient, as well as his meticulous collection and plotting of data, that led to his discovery of the source of the cholera outbreak (Vachon, 2005). Notice the relationship to the DIKW (data, information, knowledge, and wisdom) paradigm: Data were collected and interpreted (information), and knowledge was generated that led to a wise decision (wisdom).
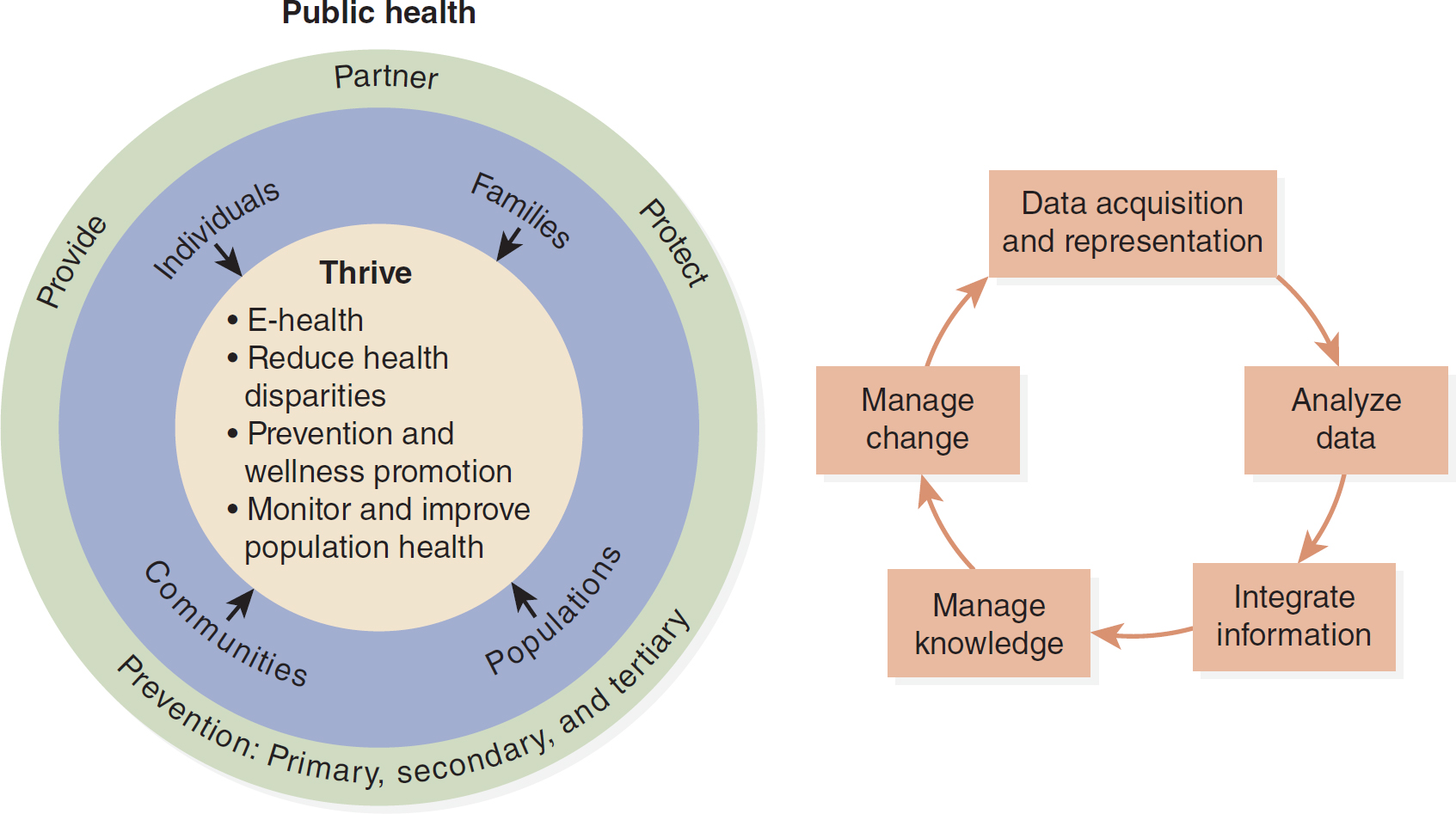
Figure 17-2 Public Health Informatics
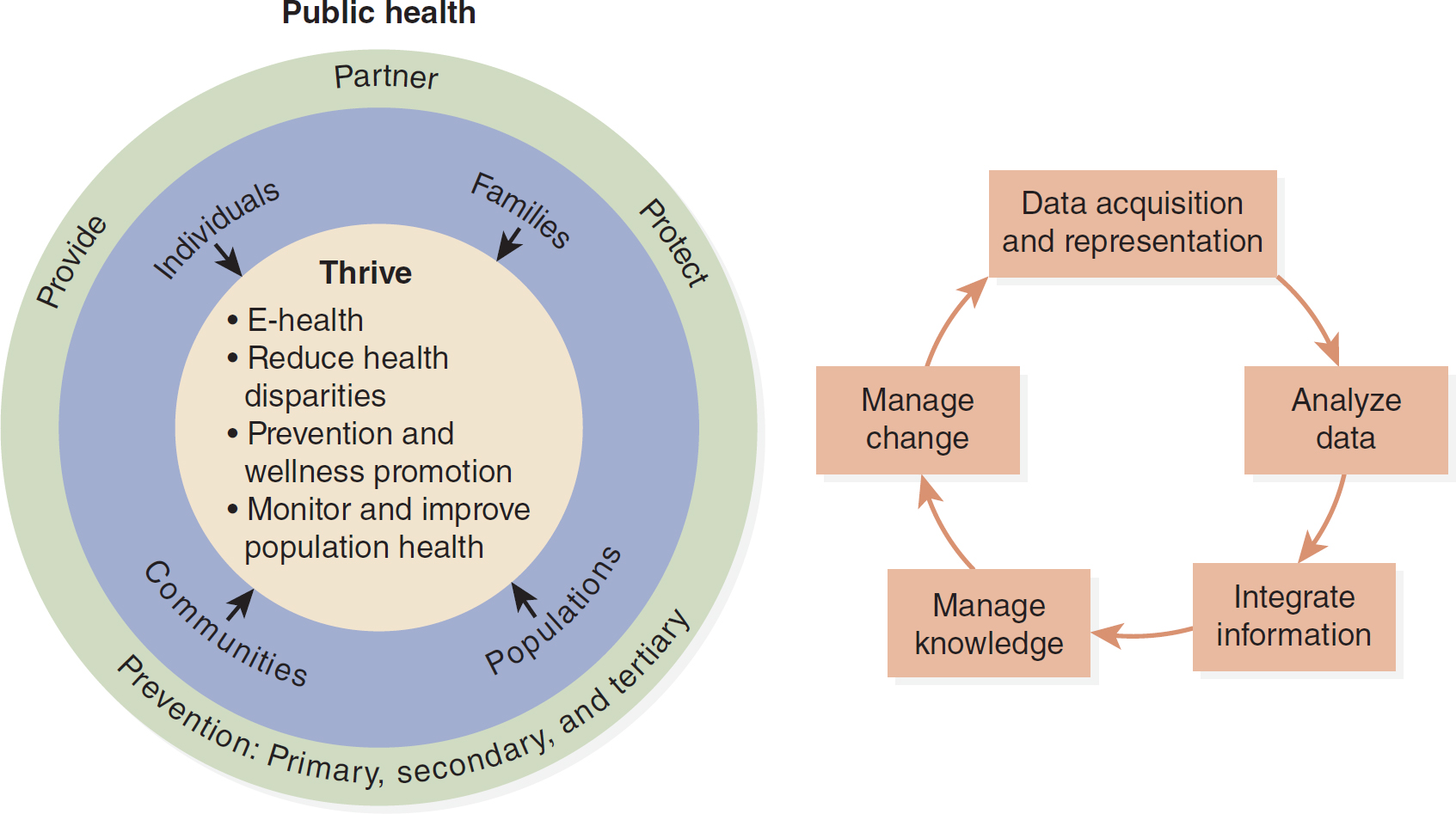
A two-part illustration depicts the concept of public health informatics.
In the first part, three nested circles outline key goals: Thrive, including E-health, reducing health disparities, prevention and wellness promotion, monitoring and improving population health; for individuals, families, populations, and communities; emphasizing the principles of provide, partner, protect, and prevention comprising primary, secondary, and tertiary. The second part features a cyclic diagram including data acquisition and representation, analysis of data, integration of information, knowledge management, and change management in public health informatics.
Florence Nightingale should also be recognized as an early public health informaticist. Her recommendations about medical reform and the need for improved sanitary conditions were based on data about morbidity and mortality that she had compiled from her experiences in Crimea and England. Her efforts led to a total reorganization of how and which healthcare statistics were collected (Dossey, 2000).
Just as information has been recognized as an asset in the business world, health care is now recognized as an information-intensive field that requires timely, accurate information from many sources. Health information systems address the collection, storage, analysis, interpretation, and communication of health data and information. Many health disciplines, such as medicine and nursing, have developed their own concepts of informatics. That trend has reached the field of public and community health. “When applied to public health, informatics can be used to enable effective monitoring and surveillance, support improved decision-making, and improve population health” (Public Health Informatics Institute, n.d.-b, para. 4). This area of informatics differs from others because it is focused on the promotion of health and disease prevention in populations and communities. PHI efficiently and effectively organizes and manages data, information, and knowledge generated and used by public health professionals to fulfill the core functions of public health: assessment, policy, and assurance. Public health changes the social conditions and systems that affect everyone within a given community. Because of public health initiatives, people understand the importance of clean water, the dangers of secondhand smoke, and that seat belts save lives. Community empowerment can be realized through the collaborative collection and analysis of data that leads to improved community health outcomes and transformed public health.
PHI addresses the data, information, and knowledge that public health professionals generate and use to meet the core functions of public health. Public health initiatives include prevention of epidemics and the spread of disease; protection against environmental hazards; promotion of health, disaster response, and recovery; and provision of access to health care. All these initiatives are dependent on quality data and information exchange. As the Public Health Informatics Institute (n.d.-b) explained,
[p]ublic health informatics assures that the right technologies are used to improve timely delivery of quality data and assists data-driven decision making. It builds bridges across siloed public health work areas by “translating” between these communities, creating opportunities for interoperable information pathways. Ultimately, public health informatics empowers disease interventions and prevention-leading to better health of individuals and the community in which they live. (para. 4)
The Integrating the Healthcare Enterprise initiative, to ensure that healthcare information can be shared more easily (using common standards) and used more effectively, has inspired the creation of the domain known as quality, research, and public health (QRPH). Participants in this domain address the repurposing of clinical, demographic, and financial data collected in the process of providing clinical care to the monitoring of disease patterns; incidence, prevalence, and situational awareness of such patterns; and identification of new patterns of disease not previously known or anticipated. Such data can be incorporated within existing public health population analyses and programs for direct outreach and condition management through registries and locally determined appropriate treatment programs or protocols (Integrating the Healthcare Enterprise, n.d.).
Community Health Risk Assessment: Tools for Acquiring Knowledge ⬆ ⬇
As the public has become more aware of harmful elements in the environment, risk assessment tools have been developed. Such tools allow assessment of pesticide use, exposure to harmful chemicals, contaminants in food and water, and toxic pollutants in the air to determine whether potential hazards need to be addressed. One such tool is the Public Health Risk Assessment Tool (PHRAT) developed by Drexel University. “The tool defines risk as the expectation of loss from a hazard and calculates risk as the product of a hazard's probability and severity, as measured by its impact across five domains: human health, health care services, inpatient health care infrastructure, community health, and public health services” (Peters et al., 2019, p. S286). Risk factor assessments provide quantitative measures of the effect of a hazard as well as adjusted risk scores, which are calculated based on the relative effect of a hazard in a subpopulation. The PHRAT also measures preparedness based on a public health agency's self-assessment of capability for emergency response and healthcare capacity. The results of the assessment are used “to prioritize planning and plan exercises for specific hazards” (p. S288), such as weather emergencies and outbreaks of infectious diseases.
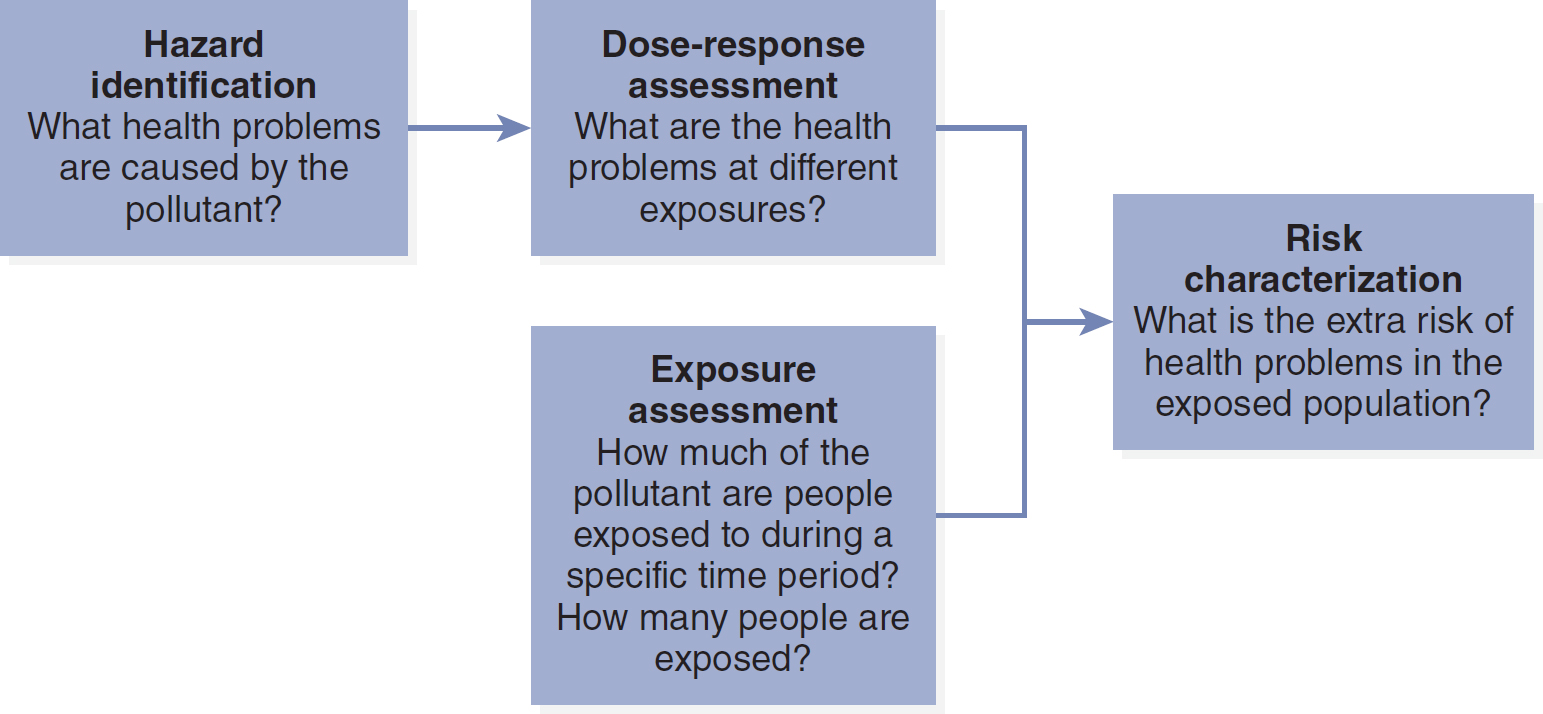
The U.S. Environmental Protection Agency (EPA; 2023a) “uses risk assessment to characterize the nature and magnitude of risks to human health for various populations-for example residents and recreational visitors, both children and adults. The EPA also estimates risks to ecological receptors, including plants, birds, other wildlife, and aquatic life” (para. 4) and to weigh the benefits and costs of various program alternatives for reducing exposure to potential hazards. It may also influence public policy and regulatory decisions. Health risk assessment is a constantly developing process, based in sound science and professional judgments. There are usually four steps ascribed to human health risk assessment (Figure 17-3):
Figure 17-3 Four-Step Risk Assessment Process
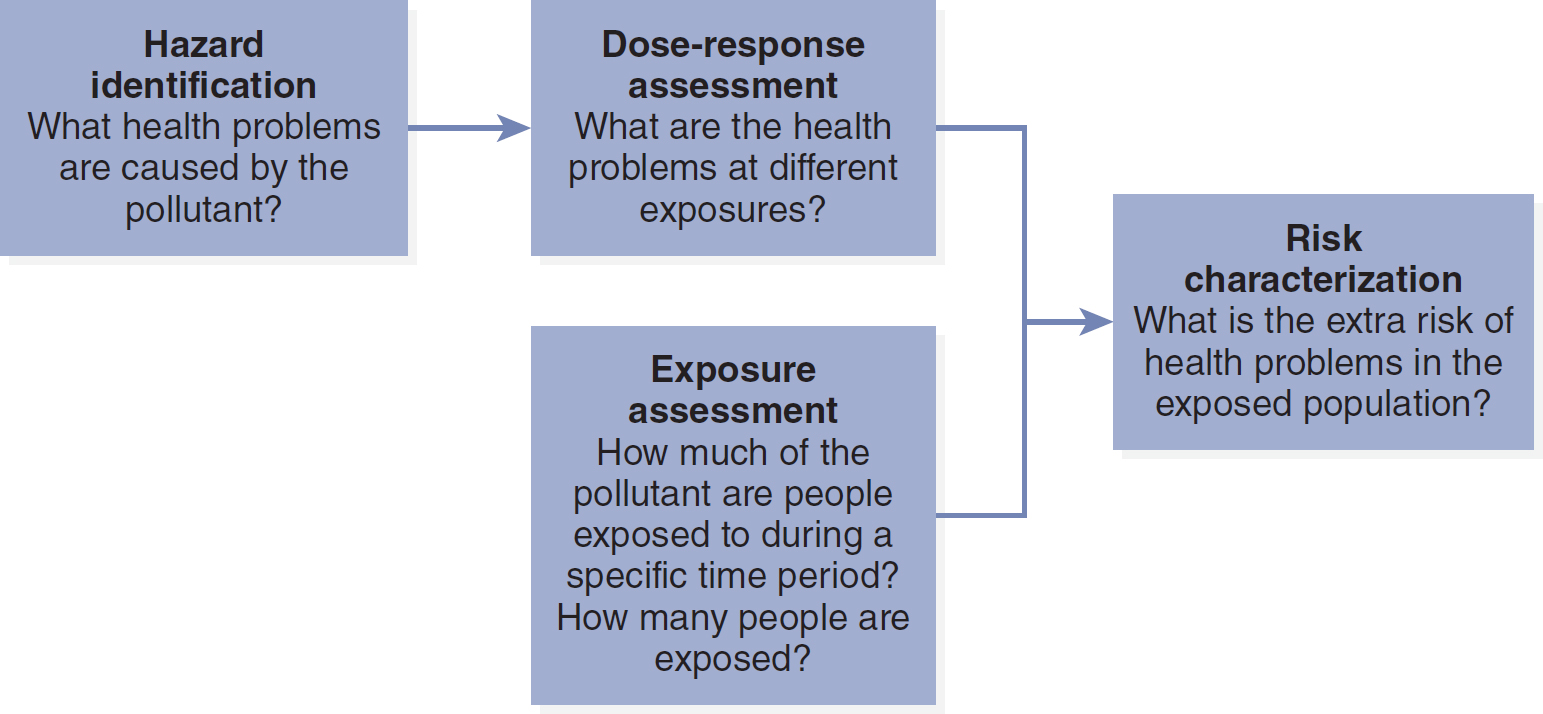
A flow diagram depicts the stages in a risk assessment process.
The stages are as follows. 1. Hazard identification: What health problems are caused by the pollutant? 2. Dose-response assessment: What are the health problems at different exposures? 3. Exposure assessment: How much of the pollutant are people exposed to during a specific time period? How many people are exposed? 4. Risk characterization: What is the extra risk of health problems in the exposed population?
Modified from: U.S. Environmental Protection Agency. (2016). Conducting a human health risk assessment. www.epa.gov/risk/conducting-human-health-risk-assessment.
- Hazard identification examines whether a stressor has the potential to cause harm to humans and/or ecological systems and, if so, under what circumstances.
- Dose-response assessment examines the numerical relationship between exposure and effects.
- Exposure assessment examines what is known about the frequency, timing, and levels of contact with a stressor.
- Risk characterization examines how well the data support conclusions about the nature and extent of the risk from exposure to environmental stressors. (EPA, 2023b, para. 2)
The overall question the risk assessment must answer is, “How much risk is acceptable?” Risk factor systems are used throughout the United States and may be local, regional, or national in scope. Specific risk assessment tools exist for specific health issues, such as the Suicide Prevention Community Assessment Tool, which addresses general community information, prevention networks, and the demographics of the target population and community assets and risk factors. Other risk assessment tools include the Youth Risk Behavior Surveillance System, Behavioral Risk Factor Surveillance System, and National Health and Nutrition Examination Survey.
Determining the presence of risk factors in a community is a key part of a community risk assessment (CRA). Communities may be concerned about which elements in the environment affect or may affect the community's health, the level of environmental risk, and other factors that should be included in public health planning. The value of a CRA derives from its ability to provide information crucial to planning, build consensus regarding how to mobilize community resources, and allow for comparison of risks with those of other communities. The goal of a CRA is risk reduction and improved health. A CRA may identify unmet needs and opportunities for action, which may help set new priorities for local public health units. It may also be used to monitor the effect of prevention programs.
Processing Knowledge and Information to Support Epidemiology and Monitoring Disease Outbreaks ⬆ ⬇
There is a need to define the role of federal, state, and local public health agencies in the development of PHI and IT applications. The availability of IT today challenges all stakeholders in the health of the public to adopt new systems that can provide adequate disease surveillance; it also challenges people to improve outmoded processes.
Preparedness in public health requires more timely detection of potential health threats, situational awareness, surveillance, outbreak management, countermeasures, response, and communications. Surveillance uses health-related data that signal a sufficient probability of a case or an outbreak that warrants further public health response. Historically, although syndromic surveillance has been used to target investigations of potential infectious cases, its use to detect possible outbreaks associated with bioterrorism is increasingly being explored by public health officials (CDC, 2018a). Early detection of possible outbreaks can be achieved through timely and complete receipt, review, and investigation of disease case reports; by improving the ability to recognize patterns in data that may be indicative of a possible outbreak early in its course; and through receipt of new types of data that can signify an outbreak earlier in its course. Such new types of data might include identification of absences from work or school; increased purchases of healthcare products, including specific types of over-the-counter medications; presenting symptoms to healthcare providers; and laboratory test orders. The University of Pittsburgh's Real-time Outbreak and Disease Surveillance Laboratory (RODS), for example, developed the National Retail Data Monitor (NRDM) system. The NRDM collects data on over-the-counter medications and other healthcare products from 28,000 stores and uses computer algorithms to detect unusual purchase patterns that might potentially signal a disease outbreak (RODS Laboratory, 2020). Keshavamurthy et al. (2022) described the use of infectious disease (ID) prediction models using artificial intelligence (AI) and machine learning processes to provide early warning in disease outbreaks. “By combining robust data collection at the speed of relevance, engineering, and analytic strategies, models can now predict disease event information, such as location, timing, intensity, and the influence of various factors responsible for its occurrence, which can be used to effectively mitigate ID impacts” (pp. 1-2). A comprehensive surveillance effort supports timely investigation and identifies data needs for managing the public health response to an outbreak or a terrorist event. Informatics tools are becoming increasingly important in these public health efforts.
To appropriately process public health data, PHI needs a standardized vocabulary and coding structure. This is especially important as national public health data are collected and data mining performed so that data variables can be understood across systems and between agencies. Health information organizations (HIOs) have been established to support data sharing via health information exchanges (HIEs), as promoted by the meaningful use criteria of the EHR. Central to these initiatives is the need for standardized codes and terminologies that may be used by the HIOs to map data from disparate sources (Hyde et al., 2013; Shapiro et al., 2011). The CDC's Public Health Information Network (PHIN) promotes semantic interoperability and secure data exchange among public health information systems. Among the tools and resources managed by this CDC (2022b) division are the following:
- PHIN Vocabulary Access and Distribution System (PHIN VADS)
- PHIN Messaging System
- PHIN Public Health Directory (PHIN DIR)
- PHIN Vocabulary Standards (para. 3-4)
Learn more about these critical initiatives by visiting www.cdc.gov/phin/index.html. In the early 1990s, the CDC launched a plan for an integrated surveillance system that moved from stand-alone systems to networked data exchange built with specific standards. These early initiatives have evolved into a comprehensive system for the collection, processing, and sharing of public health data.
Certainly, the events of September 11, 2001, indicated the need for the United States to increase its efforts directed toward prevention of terrorism and accelerated the need for informatics in public health practice. Today, response requirements include fast detection, science, communication, integration, and action. In 2005, the CDC created the National Center for Public Health Informatics (NCPHI) to provide leadership in the field. This center has since evolved into the Division of Health Informatics and Surveillance (DHIS). The DHIS manages two comprehensive public health surveillance systems, the National Notifiable Diseases Surveillance System (NNDSS) and the National Syndromic Surveillance Program (NSSP), and a data hub for research, the CDC Data Hub. It also develops information systems to support data collection exchange and processing. DHIS's stated mission is to “[p]rovide leadership in surveillance and informatics and support CDC and its partners with state-of-the-art information systems, capacity building services, and high-quality data to guide public health decisions and actions” (CDC, 2022a, para. 2). Learn more about these important services at www.cdc.gov/csels/dhis/strategic-framework.html#Focus-Areas.
The CDC also manages several surveillance systems related to tracking and managing chronic diseases. For example, there are systems for cancer, diabetes, kidney disease, smoking, and pregnancy risk and mortality. Review these systems at www.cdc.gov/chronicdisease/data/surveillance.htm.
Information is vital to public health programming. The data processed into public health information can be obtained from administrative, financial, and facility sources. Included in this data stream may be encounter, screening, registry, clinical, laboratory, and surveillance data. Public healthcare professionals recommended that the functions of population health beyond surveillance be integrated into the EHR and the personal health record. Such an initiative might allow for population-level alerts to be sent to clinicians through these electronic record systems. Systems now being developed allow for automated syndromic surveillance of emergency department records and media surveillance, which in turn supports early detection of potential pandemic occurrences. Such systems were tested during the 2009 H1N1 flu, 2014 Ebola, and 2015 Zika outbreaks and were certainly utilized during the COVID-19 crisis to track incidence. The public health-enhanced electronic medical record can provide immediate detection and reporting of notifiable conditions. The incorporation of geographic information systems allows public health data to be mapped to specific locations, which may indicate an immediate need for intervention (CDC, 2019a; Grannis & Vreeman, 2010). Modernization of data collection and analysis systems can “engage robustly with healthcare, communicate meaningfully with the public, improve health equity, and have the means to protect and promote health” (CDC, 2023d, para. 2).
Vital statistics databases (e.g., births, deaths, and cancer diagnoses) from state and local governments are also used for public health purposes. It should be noted that databases created with public funds are public databases that are readily available for use (CDC, 2023a). Access these data via the CDC Wide-ranging ONline Data for Epidemiologic Research (CDC WONDER) program at https://wonder.cdc.gov.
The widespread implementation of EHRs is facilitating the concept of a bidirectional public health-enabled record, which can automatically send patient information alerts from the point of care to public health departments when reportable symptoms, conditions, or diseases are encountered as well as allowing public health information and recommendations for treatment to be accessible at the point of care. Kruse et al. (2018) conducted a systematic review of the literature on the effects of EHRs on population health and found that EHR use supported population health by increasing productivity of practitioners, promoting surveillance for chronic diseases and health promotion activities, and supporting more comprehensive documentation and data sharing. During the COVID-19 pandemic, Reeves et al. (2020) described how a team at one academic health center built and implemented EHR applications to help manage the pandemic. Among the tools the team built were screening protocols, EHR templates, and department-specific order panels that could be modified in real time as learning about the virus continued; reporting and analytics functions; secure communication and messaging functions; and optimizing patient-facing technologies to support telemedicine visits. The health center team concluded that “[t]he electronic health record and associated technologies are vital and requisite tools in supporting outbreak management that should be leveraged to their full potential, and we hope that our experiences in developing these tools will be helpful to other health systems facing the same challenge” (p. 16).
Potential applications of HIE to public health have been described by HealthIT.gov (2023d) and Shapiro et al. (2011). These applications include syndromic surveillance using data generated from mandated and nonmandated laboratory results, physician diagnoses, and emergency or clinic chief complaints; strategies to locate loved ones in mass-casualty events; and public health alerts at the individual and population levels. There were three main types of HIE identified by HealthIT.gov (2023b):
- Directed exchange is used by a provider to send secure patient information to another provider.
- Query-based exchange allows a provider to search for health information on a patient in an unplanned healthcare encounter, such as an emergency room visit.
- Consumer-mediated exchange allows patients to securely manage their information online and share it as they choose. (para. 1)
HIE supported by an EHR resulted in better reporting rates for notifiable diseases (e.g., sexually transmitted infections and hepatitis): “The results of the study indicate that electronic, pre-populated case reporting forms integrated into providers' EHR systems and workflow, enabled by an interoperable HIE network, can be effective at increasing clinic reporting rates” (Dixon et al., 2019, para. 10).
Applying Knowledge to Health Disaster Planning and Preparation ⬆ ⬇
The availability of data and the speed of data exchange can have a significant effect on critical public health functions, such as disease detection and monitoring, syndromic surveillance, timely intervention, and overall public health planning. PHI makes real-time surveillance data available electronically, and investigations and emergencies can be managed with the tools of informatics. Surveillance data systems, such as infectious disease trackers, which collect data on adverse health effects, are invaluable tools for public health officials to tap for planning, evaluation, or implementation of public health interventions. The Agency for Toxic Substances and Disease Registry (ATSDR), for example, is a federal agency that acts as a repository for research and data regarding hazardous materials. It serves the public “by responding to environmental health emergencies; investigating emerging environmental health threats; conducting research on the health impacts of hazardous waste sites; and building capabilities of and providing actionable guidance to state and local health partners” (ATSDR, 2023, para. 1). Prior to the 2009 H1N1 pandemic, there was no common infrastructure to respond to pandemics, but the development of health IT is creating opportunities that go far beyond national boundaries to affect global public health initiatives. In May 2017, the WHO released an updated report (previous versions were released in 2009 and 2013) titled “Pandemic Influenza Risk Management,” with the goal of informing and harmonizing national and international pandemic preparedness and response. In a similar vein, the U.S. Department of Health and Human Services (2017) released a pandemic influenza plan designed to direct planning for 10 years. The plan detailed seven domains for action:
- Surveillance, Epidemiology, and Laboratory Activities
- Community Mitigation Measures
- Medical Countermeasures: Diagnostic Devices, Vaccines, Therapeutics, and Respiratory Devices
- Health Care System Preparedness and Response Activities
- Communications and Public Outreach
- Scientific Infrastructure and Preparedness
- Domestic and International Response Policy, Incident Management, and Global Partnerships and Capacity Building (pp. 5-6)
In New York City, a primary care information project, funded by the CDC, developed a multifaceted initiative, the Center of Excellence in Public Health Informatics, to address issues of measurement of meaningful use, disease and outbreak surveillance, and decision support alerts at the point of care (Hripcsak, n.d.). As a result of the continued learning prompted by the COVID-19 pandemic, we can expect to see even more knowledge tools being developed and shared in the near future.
Informatics Tools to Support Communication and Dissemination ⬆ ⬇
The revolution in IT has made the capture and analysis of health data and distribution of healthcare information more achievable and less costly. Since the early 1960s, the CDC has used IT in its practice, and PHI emerged as a specialty in the 1990s. PHI has become more important with improvements in IT; changes in the care delivery system; and the challenges related to emerging infections, resistance to antibiotics, and the threat of chemical and biological terrorism. Two-way communication between public health agencies and community and clinical laboratories can identify clusters of reportable and unusual diseases. In turn, health departments can consult on case diagnosis and management, alerts, surveillance summaries, and clinical and public health recommendations. Ongoing healthcare provider outreach and education and 24-hour access to public health professionals may lead to the discovery of urgent health threats. The automated transfer of specified data from a laboratory database to a public health data repository improves the timeliness and completeness of reporting notifiable conditions.
Public health information systems represent a partnership of federal, state, and local public health professionals. Such systems facilitate the capture of large amounts of data, rapid exchange of information, and strengthened links among these three system levels. Dissemination of prevention guidelines and communication among public health officials, clinicians, and patients have emerged as major benefits of PHI. IT solutions can be used to provide accurate and timely information that guides public health actions. In addition, the internet has become a universal communications pathway and allows individuals and population groups to be more involved and to take greater responsibility for management of their own health status. Ghio et al. (2021) conducted a systematic review to gather evidence of quality public health messaging. They emphasized that
[m]iscommunication or contradictions can result in lower compliance of preventative behaviours. Literacy is fundamental to the understanding and acceptance of any public health messaging campaign. Therefore, public health messaging should focus on clarity, simplicity, transparency and unified messaging even if tailoring to different groups regardless of the level of literacy. Even when the message is understood, different populations have different barriers to address in order to change behaviour. (p. 6)
The COVID-19 pandemic has sparked innovation in the use of informatics tools for managing the health system's response to the outbreak. As Raths (2020) reported, “In an April 9 AMIA [American Medical Informatics Association] presentation, executives describ[ed] the role clinical informatics is playing in the rapid switch to virtual care as well as public health data sharing and the creation of dashboards and registries. A common theme was that the rapid spin-up of solutions was possible because of years of work creating the informatics framework and developing standards” (para. 1). Here are examples of some of the innovations reported during the pandemic: Artificial intelligence tools have been used to screen lung scans for evidence of COVID-19-specific lung lesions and predict outbreak hot spots and resurgence by analyzing HIE and social media data; AI-based chatbots have been used to screen and triage callers to health systems after hospital lines were unable to keep up with calls; robots, facial thermal scan cameras, and no-contact infrared sensor systems were used for temperature screening to detect people with fevers and prevent or triage for hospital visits; and many systems have ramped up their use of telehealth both in and outside the hospital to minimize face-to-face interactions and save scarce personal protective equipment (McCall, 2020; Wittbold et al., 2020). As Wittbold et al. summarized, “While we race to dampen the virus's spread, we can optimize our response mechanisms, digitizing as many steps as possible. This is because traditional processes-those that rely on people to function in the critical path of signal processing-are constrained by the rate at which we can train, organize, and deploy human labor” (para. 8). Stay tuned for a literal digital transformation of health care in response to this pandemic. Now more than ever, we will need informatics-trained public health professionals.
Few long-term public health professionals have received formal informatics training. There is evidence, however, that informatics competency is increasingly emphasized in academic programs that prepare public health practitioners (Wholey et al., 2018). Public health practitioners are dependent on data and information to inform and perform their practice. In 2016, the Public Health Informatics Institute (n.d.-a) published the Applied Public Health Informatics Competency model, which “frames the knowledge, skills, and abilities that public health practitioners need to address the informatics challenges at their agencies” (p. 2). Key components of this model include the following:
- Principles and Strategy: Ability to apply informatics principles and strategic thinking to public health information needs, ensuring organizational strategic alignment.
- Standards and Interoperability: Applies informatics standards to ensure interoperability between disparate information systems.
- Project Management: Practices project management techniques to engage stakeholders and achieve needs and expectations.
- Information Systems: Fundamental knowledge of hardware, software and network infrastructure essential to ensuring that public health requirements are met.
- Communication: Practices active, effective communication between IT, public health and other relevant stakeholders.
- Evaluation: Applies rigorous methods to evaluate the effectiveness of workflows and information technology.
- Analysis, Visualization, and Reporting (AVR): Translates data to information and knowledge that leads to action.
- Policy: Ensures that information projects adhere to relevant laws, rules and regulations. (pp. 3-10)
Access the full model here for explanatory statements related to each of the competencies listed: https://phii.org/wp-content/uploads/2021/06/Applied-Public-Health-Informatics-Competency-Model.pdf.
Using Feedback to Improve Responses and Promote Readiness ⬆ ⬇
Improvement of community health status and population health depends on effective public and healthcare infrastructures. In addition to information from public health agencies, there is now interest in the capture of information from hospitals, pharmacies, poison control centers, laboratories, and environmental agencies. Timely collection of such data allows for early detection and analysis, which can increase the rapidity of response with more effective interventions. Great strides have been made toward a national public health information system, but informaticists currently are still striving to make this a reality. Initially, there was a 10-year vision to achieve an interoperable health IT infrastructure in the United States (HealthIt.gov, 2014). In 2022, the Office of the National Coordinator for Health Information Technology (2022) released the 2022 Interoperability Standards Advisory: www.healthit.gov/isa/sites/isa/files/inline-files/2022-ISA-Reference-Edition.pdf. We have yet to fully achieve the 10-year interoperability goal.
Population health data must be considered an important part of the infrastructure of all regional health information exchanges, which are the building blocks for a national health information network. Organizations and agencies interested in promoting and protecting the public's health must commit to collaboration and seamless data sharing (HealthIt.gov, 2014). Public health data include data related to surveillance, environmental health, and preparedness systems as well as client information, such as data from immunization registries and laboratory results reporting and analysis. These types of data can provide information about outbreaks, patterns of drug-resistant organisms, and other trends that can help improve the accuracy of diagnostic and treatment decisions and advance public health research (National Institutes of Health, n.d.). A regional HIE and national health information network can also support public health goals through broader opportunities for participation in surveillance and prevention activities, improved case management and care coordination, and increased accuracy and timeliness of information for disease reporting. In 2019, HealthIT.gov released the second draft of the Trusted Exchange Framework and Common Agreement (TEFCA) and, in 2022, the Qualified Health Information Network framework (QHIN) to promote electronic health information exchange across disparate systems. For more complete information about the TEFCA, access the user's guide here: www.healthit.gov/sites/default/files/page/2019-04/TEFCADraft2UsersGuide.pdf.
Much public health information is focused on reaction to issues and timely intervention rather than on harnessing information technology for disease prevention. As early as 2011, Fuller advocated for a shift to prevention informatics by harnessing real-time social data and aggregating and representing these data in a meaningful way so that an appropriate prevention response can be mounted. For example, internet searches related to flu symptoms might prompt a public health prevention response, such as a school closure, to minimize spread. A software tool that supports mapping and real-time data visualization is Ushahidi, which supports “gathering of distributed data from the web and other data streams” (Fuller, 2011, p. 40). “Prevention informatics offers a useful paradigm for re-imagining health information systems and for harnessing the vast array of data, tools, technologies and systems to respond proactively to health challenges across the globe” (Fuller, 2011, p. 41).
Harnessing data from social media, such as X (Twitter) and Facebook, provides yet another example of using citizen-generated information (i.e., crowdsourcing) in community health. Merchant et al. (2011) described how mining data generated in social media can improve the response to mass disasters by helping responders locate people who require help and identifying areas that need resources, building social capital, and promoting community resilience after the disaster. “Tweets and photographs linked to timelines and interactive maps can tell a cohesive story about a recovering community's capabilities and vulnerabilities in real time” (Merchant et al., 2011, p. 291). These authors cautioned, however, that social media should be used to augment-not replace-current disaster response and communication systems because not all communications in social media are entirely trustworthy. In addition to utilizing social media posts, Benforado's (2015) presentation to the EPA on Citizen Science and Crowdsourcing asked the question, “If you had 100,000 people to help you with your work, what would you do?” (slide 2). Enlisting and empowering people can promote volunteerism and advance science. There is power in investing in citizen science approaches and harnessing the efforts of volunteers. The use of social media data during public emergencies has been variously termed crisis informatics or disaster informatics. Palen and Anderson (2016) suggested that social media use is important during disaster response because it gives people affected by the disaster a voice and a means to participate in a response.
Reuter and Kaufhold (2018) identified four types of communication capability via social media during a crisis: citizen to citizen (C2C), authorities to citizens (A2C), citizens to authorities (C2A), and authorities to authorities (A2A). Further, they argued that not all social media use during a disaster or crisis is positive, especially in the case of dissemination of false or misleading information. They concluded that “[t]rust is the main issue, so future work might focus on the key enablers, like positive examples of social media use. The feeling to be part of a movement that productively works together to overcome crises and emergencies is the intended result of this” (p. 52). Basch et al. (2022) stated, “Our work indicates that the content of official public health agency social media accounts does not receive as many views as communications posted by popular entertainers, influencers, or, in some cases, even consumers. Partnerships with carefully vetted content creators may help to extend the reach of accurate health information on social media, particularly to young people who tend to use these platforms in higher numbers than older adults” (pp. 3-4). The use of social media during the COVID-19 pandemic increased exponentially. However, the credibility of the information that is crowdsourced is difficult to discern. During a crisis, it is best to seek information from credible sources, such as the CDC. The CDC can be followed on various social media, such as Facebook, Twitter, and YouTube. It has a comprehensive toolkit guiding the use of social media. Access the Social Media Toolkit here: www.cdc.gov/healthcommunication/toolstemplates/socialmediatoolkit_bm.pdf.
Summary ⬆ ⬇
PHI strives to ensure that evolving health data systems will meet the data needs of all organizations interested in population health as national and international standards are developed for healthcare data collection. The data included in this standardization process are environmental, sociocultural, economic, and other data that are relevant to public health. As a result of the COVID-19 pandemic, PHI will likely garner more widespread appreciation and respect as well as creative innovation that will affect public health initiatives for years to come. Table 17-1 provides the names, addresses, and URLs for important organizations dedicated to public health data and informatics.
Table 17-1 Important PHI SitesName | Address | Website |
|---|
American Public Health Association | 800 I Street NW, Washington, DC 20001 | www.apha.org |
Centers for Disease Control and Prevention | 1600 Clifton Road, Atlanta, GA 30333 | www.cdc.gov |
AHIMA Public Health Data Standards Council | 233 N. Michigan Avenue, 21st Floor, Chicago, IL 60601-5809 | www.ahima.org |
Public Health Institute | 555 12th Street, 10th Floor, Oakland, CA 94607 | www.phi.org |
The future of practice in public health depends on how efficiently and effectively public health data are captured, analyzed, and disseminated for regional, national, and global health planning and management. In an ideal world, we would see seamless data collection and sharing with a commitment to prevention and global health planning.
| Thought-Provoking Questions |
|---|
- Imagine that you are a PHI specialist and that you and your colleagues are concerned about the response to the COVID-19 pandemic. Review the public health data that were used to determine the response to the pandemic. Which data would need to be collected to assess the outcomes of the pandemic response?
- What are the advantages and disadvantages of using crowdsourced social media data during a disaster response?
- Choose an informatics tool that was developed or modified during the COVID-19 pandemic. Assess its long-term sustainability.
|
References ⬆
- Agency for Toxic Substances and Disease Registry. (2023). Home page.www.atsdr.cdc.gov
- Basch C. H., Basch C. E., Hillyer G. C., & Meleo-Erwin Z. C. (2022). Social media, public health, and community mitigation of COVID-19: Challenges, risks, and benefits. Journal of Medical Internet Research, 24(4), e36804. https://doi.org/10.2196/36804
- Benforado J. (2015 December 1). Citizen science and crowdsourcing. Environmental Protection Agency. www.epa.gov/sites/production/files/2016-02/documents/citizen-science-crowdsourcing.pdf
- CDC Foundation. (n.d.). What is public health? www.cdcfoundation.org/content/what-public-health
- Centers for Disease Control and Prevention. (2015). Information about Middle East respiratory syndrome (MERS). www.cdc.gov/coronavirus/mers/downloads/factsheet-mers_en.pdf
- Centers for Disease Control and Prevention. (2017). Severe acute respiratory syndrome (SARS). www.cdc.gov/sars/index.html
- Centers for Disease Control and Prevention. (2018a). Emergency preparedness and response: Video: “The history of bioterrorism.”http://emergency.cdc.gov/training/historyofbt/index.asp
- Centers for Disease Control and Prevention. (2018b). Influenza (flu): Past flu pandemics. www.cdc.gov/flu/pandemic-resources/basics/past-pandemics.html
- Centers for Disease Control and Prevention. (2019a). Division of Health Informatics and Surveillance: DHIS overview. https://www.cdc.gov/csels/dhis/overview.html
- Centers for Disease Control and Prevention. (2022a). Division of Health Informatics and Surveillance: DHIS strategic framework. www.cdc.gov/csels/dhis/strategic-framework.html#Focus-Areas
- Centers for Disease Control and Prevention. (2022b). PHIN tools and resources. www.cdc.gov/phin/index.html
- Centers for Disease Control and Prevention. (2022c). Surveillance Resource Center.www.cdc.gov/surveillancepractice/index.html
- Centers for Disease Control and Prevention. (2022d). Zika virus. www.cdc.gov/zika
- Centers for Disease Control and Prevention. (2023a). CDC WONDER. https://wonder.cdc.gov
- Centers for Disease Control and Prevention. (2023b). FAQ: COVID-19 data and surveillance. www.cdc.gov/coronavirus/2019-ncov/covid-data/faq-surveillance.html
- Centers for Disease Control and Prevention. (2023c). Public health professionals gateway: 10 essential public health services. www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html
- Centers for Disease Control and Prevention. (2023d). Public health surveillance and data: Data Modernization Initiative. www.cdc.gov/surveillance/surveillance-data-strategies/data-IT-transformation.html
- Correll R. (2022, August 28). The 10 essential public health services. Verywell Health. www.verywellhealth.com/essential-public-health-services-4150535
- Dixon B. E., Grannis S. J., & Gibson J. (2019). Enhancing provider reporting of notifiable diseases using HIE-enabled decision support. Online Journal of Public Health Informatics, 11(1). https://doi.org/10.5210/ojphi.v11i1.9706
- Dossey B. M. (2000). Florence Nightingale: Mystic, visionary, healer. Springhouse.
- Felman A. (2021, Feburary 1). What to know about coronaviruses. Medical News Today. www.medicalnewstoday.com/articles/256521
- Fuller S. (2011). From intervention informatics to prevention informatics. Bulletin of the American Society for Information Science & Technology, 38(1), 36-41. https://doi.org/10.1002/bult.2011.17,20380112
- Ghio D., Lawes-Wickwar S., Tang M. Y., Epton T., Howlett N., Jenkinson E., Stanescu S., Westbrook J., Kassianos A. P., Watson D., Sutherland L., Stanulewicz N., Guest E., Scanlan D., Carr N., Chater A., Hotham S., Thorneloe R., Armitage C. J., . . . Keyworth C. (2021). What influences people's responses to public health messages for managing risks and preventing infectious diseases? A rapid systematic review of the evidence and recommendations. BMJ Open, 11(11), e048750. doi.org/10.1136/bmjopen-2021-048750
- Grannis S., & Vreeman D. (2010). A vision of the journey ahead: Using public health notifiable condition mapping to illustrate the need to maintain value sets. AMIA Annual Symposium Proceedings, 2010, 261-265. www.ncbi.nlm.nih.gov/pmc/articles/PMC3041316
- HealthIt.gov. (2014). Connecting health and care for the nation: A 10-year vision to achieve an interoperable health IT infrastructure. www.healthit.gov/sites/default/files/ONC10yearInteroperabilityConceptPaper.pdf
- HealthIT.gov. (2023a). Improving public and population health outcomes. www.healthit.gov/faq/how-can-electronic-health-records-improve-public-and-population-health-outcomes
- HealthIT.gov. (2023b). The three key forms of health information exchange.www.healthit.gov/faq/what-are-different-types-health-information-exchange
- HealthIT.gov. (2023d). What is HIE?www.healthit.gov/topic/health-it-and-health-information-exchange-basics/what-hie
- Hickok K. (2020, March 18). How does the COVID-19 pandemic compare to the last pandemic? Live Science. www.livescience.com/covid-19-pandemic-vs-swine-flu.html
- Hripcsak G. (n.d.). NYC Center of Excellence for Public Health Informatics. http://grantome.com/grant/NIH/P01-HK000029-03
- Hyde L., Rihanek T., Santana-Johnson T., Scichilone R., Simmons C., Turner J. B., & Zumar W. (2013). Data mapping and its impact on data integrity. American Health Information Management Association. http://library.ahima.org/PdfView?oid=107154
- Integrating the Healthcare Enterprise. (n.d.). Quality, research and public health. www.ihe.net/ihe_domains/quality_research_and_public_health
- Keshavamurthy R., Dixon S., Pazdernik K. T., & Charles L. E. (2022). Predicting infectious disease for biopreparedness and response: A systematic review of machine learning and deep learning approaches. One Health, 15, 100439. https://doi.org/10.1016/j.onehlt.2022.100439
- Klobucista C., & Renwick D. (2020, July 1). What is the Ebola virus? Council on Foreign Relations. www.cfr.org/backgrounder/ebola-virus
- Kruse C. S., Stein A., Thomas H., & Kaur H. (2018). The use of electronic health records to support population health: A systematic review of the literature. Journal of Medical Systems, 42(214), 1-16. https://doi.org/10.1007/s10916-018-1075-6
- Lee B., Martin T., Khan A., Fullerton K., Duck W., Kinley T., Stoutenburg S., Hall J., Crum M., Garcia M. C., Iademarco M. F., & Richards C. L. (2018). Modernizing Centers for Disease Control and Prevention informatics using surveillance data platform shared services. Public Health Reports, 133(2), 130-135. https://doi.org/10.1177/0033354917751130
- McCall B. (2020). COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. Lancet Digital Health, 2(4), e166-e167. https://doi.org/10.1016/S2589-7500(20)30054-6
- Merchant R., Elmer S., & Lurie N. (2011). Integrating social media into emergency-preparedness efforts. New England Journal of Medicine, 365, 289-291. http://dx.doi.org/10.1056/NEJMp1103591
- Modjarrad K., Moorthy V. S., Millett P., Gsell , P.-S., Roth C., & Kieny , M.-P. (2016). Developing global norms for sharing data and results during public health emergencies. PLoS Medicine, 13(1), e1001935. https://doi.org/10.1371/journal.pmed.1001935
- National Institutes of Health. (n.d.). Health data resources: Common data types in public health research. www.nihlibrary.nih.gov/resources/subject-guides/health-data-resources/common-data-types-public-health-research
- Office of the National Coordinator for Health Information Technology. (2022). 2022 interoperability standards advisory, reference edition.www.healthit.gov/isa/sites/isa/files/inline-files/2022-ISA-Reference-Edition.pdf
- Palen L., & Anderson K. M. (2016). Crisis informatics-New data for extraordinary times. Science, 353(6296), 224-225. http://dx.doi.org/10.1126/science.aag2579
- Peters R., Hipper T. J., Kricun H., & Chernak E. (2019). A quantitative public health risk assessment tool for planning for at-risk populations. American Journal of Public Health, 109(S4), S286-S289. https://doi.org/10.2105/AJPH.2019.305181
- Public Health Informatics Institute. (n.d.-a). Applied public health informatics competency model. https://phii.org/wp-content/uploads/2021/06/Applied-Public-Health-Informatics-Competency-Model.pdf
- Public Health Informatics Institute. (n.d.-b). INFOR-WHAT-ICS? Defining public health informatics. www.phii.org/defining-public-health-informatics
- Raths D. (2020, April 10). COVID-19 preparedness: “Every answer touches clinical informatics in some way or another.” Healthcare Innovation. www.hcinnovationgroup.com/clinical-it/workflow/article/21133486/covid19-preparedness-every-answer-touches-clinical-informatics-in-some-way-or-another
- Reeves J., Hollandsworth H., Torriani F., Taplitz R., Abeles S., Tai-Seale M., Millen M., Clay B., & Longhurst C. (2020). Rapid response to COVID-19: Health informatics support for outbreak management in an academic health system. Journal of the American Medical Informatics Association, 27(6), 853-859. http://dx.doi.org/10.1093/jamia/ocaa037
- Reuter C., & Kaufhold M. (2018). Fifteen years of social media in emergencies: A retrospective review and future directions for crisis informatics. Journal of Contingencies and Crisis Management, 26(1), 41-57. http://dx.doi.org/10.1111/1468-5973.12196
- RODS Laboratory. (2020). About the National Retail Data Monitor. www.rods.pitt.edu/content/blogsection/4/42/index.html
- Shapiro J. S., Mostashari F., Hripcsak G., Soulakis N., & Kuperman G. (2011). Using health information exchange to improve public health. American Journal of Public Health, 101(4), 616-623. http://dx.doi.org/10.2105/AJPH.2008.158980
- U.S. Department of Health and Human Services. (2017). Pandemic influenza plan: 2017 update. www.cdc.gov/flu/pandemic-resources/pdf/pan-flu-report-2017v2.pdf
- U.S. Environmental Protection Agency. (2016). Conducting a human health risk assessment. www.epa.gov/risk/conducting-human-health-risk-assessment
- U.S. Environmental Protection Agency. (2023a). About risk assessment. www.epa.gov/risk/about-risk-assessment
- U.S. Environmental Protection Agency. (2023b). Human health risk assessment. www.epa.gov/risk/human-health-risk-assessment
- Vachon D. (2005). Doctor John Snow blames water pollution for cholera epidemic. Old News, 16(8), 8-10. UCLA Department of Epidemiology. www.ph.ucla.edu/epi/snow/fatherofepidemiology.html
- Wholey D. R., LaVenture M., Rajamani S., Kreiger R., Hedberg C., & Kenyon C. (2018). Developing workforce capacity in public health informatics: Core competencies and curriculum design. Frontiers in Public Health, 6. http://dx.doi.org/10.3389/fpubh.2018.00124
- Wittbold K., Carroll C., Iansiti M., Zhang H., & Landman A. (2020, April 3). How hospitals are using AI to battle Covid-19. Harvard Business Review. https://hbr.org/2020/04/how-hospitals-are-using-ai-to-battle-covid-19
- World Health Organization. (2017). Pandemic influenza risk management: A WHO guide to inform and harmonize national and international pandemic preparedness and response. https://apps.who.int/iris/handle/10665/259893
- World Health Organization. (2021). World Health Organization declares SARS contained worldwide. www.history.com/this-day-in-history/world-health-organization-declares-sars-contained-worldwide