A Look at AV Block
AV heart block results from an interruption in the conduction of impulses between the atria and ventricles. AV block can be total or partial or it may delay conduction. The block can occur at the AV node, the bundle of His, or the bundle branches.
The heart’s electrical impulses normally originate in the sinoatrial (SA) node, so when those impulses are blocked at the AV node, atrial rates are commonly normal (60 to 100 beats/min). The clinical effect of the block depends on how many impulses are completely blocked, how slow the ventricular rate is as a result, and how the block ultimately affects the heart. A slow ventricular rate can decrease cardiac output, possibly causing light-headedness, hypotension, and confusion.

The Cause Before the Block
Various factors can lead to AV block, including underlying heart conditions, use of certain drugs, congenital anomalies, and conditions that disrupt the cardiac conduction system. (See Causes of AV block)
Typical examples include
- myocardial ischemia, which impairs cellular function so cells repolarize more slowly or incompletely. The injured cells, in turn, may conduct impulses slowly or inconsistently. Relief of the ischemia can restore normal function to the AV node.
- MI, in which cell death occurs. If the necrotic cells are part of the conduction system, they no longer conduct impulses and a permanent AV block occurs.
- excessive dosage of, or an exaggerated response to, a drug that can cause AV block or increase the likelihood that a block will develop. Although many antiarrhythmic medications can have this effect, the drugs more commonly known to cause or exacerbate AV blocks include digoxin, beta-adrenergic blockers, and calcium channel blockers.
- congenital anomalies such as congenital ventricular septal defect that involve cardiac structures and affect the conduction system. Anomalies of the conduction system, such as an AV node that doesn’t conduct impulses, can also occur in the absence of structural defects. (See AV block in elderly patients.)
Under the Knife
AV block may also be caused by inadvertent damage to the heart’s conduction system during cardiac surgery. Damage is most likely to occur in surgery involving the mitral or tricuspid valve or in the closure of a ventricular septal defect. If the injury involves tissues adjacent to the surgical site and the conduction system isn’t physically disrupted, the block may be only temporary. If a portion of the conduction system itself is severed, a permanent block results.
Radio Blackout
Similar disruption of the conduction system can occur from a procedure called radiofrequency ablation. In this invasive procedure, a transvenous catheter is used to locate the area within the heart that participates in initiating or perpetuating certain tachyarrhythmias.
Radiofrequency energy is then delivered to the myocardium through this catheter to produce a small area of necrosis. The damaged tissue can no longer cause or participate in the tachyarrhythmia. If the energy is delivered close to the AV node, bundle of His, or bundle branches, block can occur.
Degrees of Block
AV blocks are classified according to their severity, not their location. That severity is measured according to how well the node conducts impulses and is separated by degrees—first, second, and third. Let’s take a look at them one at a time.
First-Degree AV Block

First-degree AV block occurs when impulses from the atria are consistently delayed during conduction through the AV node. All atrial impulses reach the ventricle; however, the conduction delay occurs within the AV node. Conduction eventually occurs; it just takes longer than normal. It’s as if people are walking in a line through a doorway, but each person hesitates before crossing the threshold.

How It Happens
First-degree AV block may appear normally in a healthy person or result from myocardial ischemia or infarction, myocarditis, or degenerative changes in the heart. The condition may also be caused by medications, such as digoxin, calcium channel blockers, and beta-adrenergic blockers.
First-degree AV block may be temporary, particularly if it stems from medications or ischemia early in the course of a MI. The presence of first-degree block, the least dangerous type of AV block, indicates some kind of problem in the conduction system.
Because first-degree AV block can progress to a more severe block, it should be monitored for changes.
What to Look for
In general, a rhythm strip with this block looks like normal sinus rhythm except that the PR interval is longer than normal. (See Identifying first-degree AV block.) The rhythm will be regular, with one normal P wave for every QRS complex.
The PR interval will be greater than 0.20 second and will be consistent for each beat. The QRS complex is usually normal, although sometimes a bundle branch block may occur along with first-degree AV block and cause a widening of the QRS complex.
No Signs of Block
Most patients with first-degree AV block show no symptoms of the block because cardiac output isn’t significantly affected. If the PR interval is extremely long, a longer interval between S1 and S2 may be noted on cardiac auscultation.
How You Intervene
Usually, just the underlying cause will be treated, not the conduction disturbance itself. For example, if a medication is causing the block, the dosage may be reduced or the medication may be discontinued. Close monitoring helps to detect progression of first-degree AV block to a more serious form of block.
When caring for a patient with first-degree AV block, evaluate them for underlying causes that can be corrected, such as medications or ischemia. Observe the ECG for progression of the block to a more severe form of block. Administer digoxin, calcium channel blockers, or beta-adrenergic blockers cautiously.
Type I Second-Degree AV Block

Also called Mobitz type I block or Wenckebach, type I second-degree AV block occurs when each successive impulse from the SA node is delayed slightly longer than the previous impulse. That pattern continues until an impulse fails to be conducted to the ventricles, and the cycle then repeats. The block generally will occur at the AV node but can also occur in the bundle of His or the Purkinje system. It’s like a line of people trying to get through a doorway, each one taking longer and longer until finally one can’t get through.

How It Happens
Causes of type I second-degree AV block include coronary artery disease, inferior wall MI, and rheumatic fever. It may also be because of cardiac medications, such as beta-adrenergic blockers, digoxin, and calcium channel blockers. Increased vagal stimulation can also cause this type of block.
Type I second-degree AV block may occur normally in an otherwise healthy person. Almost always temporary, this type of block resolves when the underlying condition is corrected. Although an asymptomatic patient with this block has a good prognosis, the block may progress to a more serious form, especially if it occurs early during a MI.
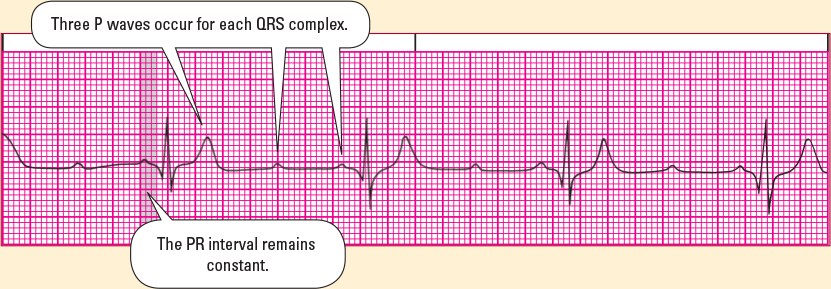
What to Look for
When monitoring a patient with type I second-degree AV block, you’ll note that because the SA node isn’t affected by this lower block, it continues its normal activity. As a result, the atrial rhythm is normal. (See Identifying type I second-degree AV block.)
The PR interval gets gradually longer with each successive beat until finally a P wave fails to conduct to the ventricles. This makes the ventricular rhythm irregular, with a repeating pattern of groups of QRS complexes followed by a dropped beat in which the P wave isn’t followed by a QRS complex.
Famous Footprints
The pattern of grouped beating is sometimes referred to as the footprints of Wenckebach. (Karel Frederik Wenckebach was a Dutch internist who, at the turn of the century and long before the introduction of the ECG, described the two forms of what’s now known as second-degree AV block by analyzing waves in the jugular venous pulse. Following the introduction of the ECG, German cardiologist Woldemar Mobitz clarified Wenckebach’s findings as type I and type II.)
As you’ve probably noticed by now, rhythm strips have distinctive patterns. (See Rhythm strip patterns.)
Lonely Ps, Light-Headed Patients
Usually asymptomatic, a patient with type I second-degree AV block may show signs and symptoms of decreased cardiac output, such as light-headedness or hypotension. Symptoms may be especially pronounced if the ventricular rate is slow.
How You Intervene
No treatment is needed if the patient is asymptomatic. For a symptomatic patient, atropine may improve AV node conduction. A temporary pacemaker may be required for long-term relief of symptoms until the rhythm resolves.
When caring for a patient with this block, assess their tolerance for the rhythm and the need for treatment to improve cardiac output. Evaluate the patient for possible causes of the block, including the use of certain medications or the presence of ischemia.
Check the ECG frequently to see if a more severe type of AV block develops. Make sure the patient has a patent IV line. Teach them about temporary pacemaker, if indicated.
Type II Second-Degree AV Block

Type II second-degree AV block, also known as Mobitz type II block, is less common than type I but more serious. It occurs when occasional impulses from the SA node fail to conduct to the ventricles.
On an ECG, you won’t see the PR interval lengthen before the impulse fails to conduct, as you do with type I second-degree AV block. You’ll see, instead, consistent AV node conduction and an occasional dropped beat. This block is like a line of people passing through a doorway at the same speed, except that, periodically, one of them just can’t get through.

How It Happens
Type II second-degree AV block is usually caused by an anterior wall MI, degenerative changes in the conduction system, or severe coronary artery disease. The arrhythmia indicates a problem at the level of the bundle of His or bundle branches.
Type II block is more serious than type I because the ventricular rate tends to be slower and the cardiac output diminished. It’s also more likely to cause symptoms, particularly if the sinus rhythm is slow and the ratio of conducted beats to dropped beats is low such as 2:1. (See 2:1 AV block.) Usually chronic, type II second-degree AV block may progress to a more serious form of block. (See High-grade AV block.)
| Don’t skip this strip |
| High-grade AV block When two or more successive atrial impulses are blocked, the conduction disturbance is called high-grade AV block. Expressed as a ratio of atrial-to-ventricular beats, this block will be at least 3:1. With the prolonged refractory period of this block, latent pacemakers can discharge. As a result, you’ll commonly see escape rhythms develop. Complications High-grade AV block causes severe complications. For instance, decreased cardiac output and reduced heart rate can combine to cause Stokes–Adams syncopal attacks. In addition, high-grade AV block usually progresses quickly to third-degree block. Look for these distinguishing characteristics:
|
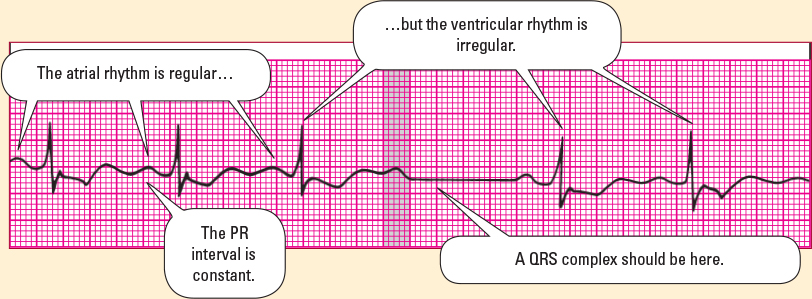
What to Look for
When monitoring a rhythm strip, look for an atrial rhythm that’s regular and a ventricular rhythm that may be regular or irregular, depending on the block. (See Identifying type II second-degree AV block) If the block is intermittent, the rhythm is irregular. If the block is constant, such as 2:1 or 3:1, the rhythm is regular.
Overall, the strip will look as if someone erased some QRS complexes. The PR interval will be constant for all conducted beats but may be prolonged. The QRS complex is usually wide, but normal complexes may occur.
Jumpin’ Palpitations!
Most patients who experience a few dropped beats remain asymptomatic as long as cardiac output is maintained. As the number of dropped beats increases, patients may experience palpitations, fatigue, dyspnea, chest pain, or light-headedness. On physical examination, you may note hypotension, and the pulse may be slow and regular or irregular.
How You Intervene
If the dropped beats are infrequent and the patient shows no symptoms of decreased cardiac output, the practitioner may choose only to observe the rhythm, particularly if the cause is thought to be reversible. If the patient is hypotensive, treatment aims to improve cardiac output by increasing the heart rate. Atropine, dopamine, or epinephrine may be given for symptomatic bradycardia. Discontinue digoxin if it’s the cause of the arrhythmia.
Because the conduction block occurs in the His–Purkinje system, transcutaneous pacing should be initiated quickly.
Pacemaker Place
Type II second-degree AV block commonly requires placement of a pacemaker. A temporary pacemaker may be used until a permanent pacemaker can be placed.
When caring for a patient with type II second-degree block, assess their tolerance for the rhythm and the need for treatment to improve cardiac output. Evaluate for possible correctable causes such as ischemia.
Keep the patient on bed rest, if indicated, to reduce myocardial oxygen demand s. Administer oxygen therapy as ordered. Observe the patient for progression to a more severe form of AV block. If the patient receives a pacemaker, teach them and their family about its use.
Third-Degree AV Block
Also called complete heart block, third-degree AV block occurs when impulses from the atria are completely blocked at the AV node and can’t be conducted to the ventricles. Maintaining our doorway analogy, this form of block is like a line of people waiting to go through a doorway, but no one can go through.

Beats of Different Drummers
Acting independently, the atria, generally under the control of the SA node, tend to maintain a regular rate of 60 to 100 beats/min. The ventricular rhythm can originate from the AV node and maintain a rate of 40 to 60 beats/min. Most typically, it originates from the Purkinje system in the ventricles and maintains a rate of 20 to 40 beats/min. The QRS complexes often resemble an escape rhythm.
The rhythm strip will look like a strip of P waves laid independently over a strip of QRS complexes. Note that the P wave doesn’t conduct the QRS complex that follows it.
How It Happens
Third-degree AV block that originates at the level of the AV node is most commonly a congenital condition. This block may also be caused by coronary artery disease, an anterior or inferior wall MI, degenerative changes in the heart, digoxin toxicity, calcium channel blockers, beta-adrenergic blockers, or surgical injury. It may be temporary or permanent. (See Heart block after congenital heart repair.)
Because the ventricular rate is so slow, third-degree AV block presents a potentially life-threatening situation because cardiac output can drop dramatically. In addition, the patient loses their atrial kick—extra 30% of blood flow pushed into the ventricles by atrial contraction. That happens as a result of the loss of synchrony between the atrial and ventricular contractions. The loss of atrial kick further decreases cardiac output. Any exertion on the part of the patient can worsen symptoms.

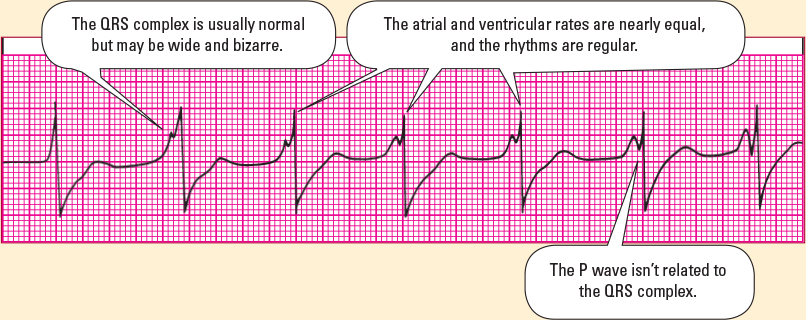
What to Look for
When analyzing an ECG for this rhythm, you’ll note that the atrial and ventricular rhythms are regular. The P and R waves can be “walked out” across the strip, meaning that they appear to march across the strip in rhythm. (See Identifying third-degree AV block.)
Some P waves may be buried in QRS complexes or T waves. The PR interval will vary with no pattern or regularity. If the resulting rhythm, called the escape rhythm, originates in the AV node, the QRS complex will be normal and the ventricular rate will be 40 to 60 beats/min. If the escape rhythm originates in the Purkinje system, the QRS complex will be wide, with a ventricular rate below 40 beats/min.
Escape!
The PR interval varies because the atria and ventricles beat independently of each other. The QRS complex is determined by the site of the escape rhythm. Usually, the duration and configuration are normal; however, with an idioventricular escape rhythm (an escape rhythm originating in the ventricles), the duration is greater than 0.12 second and the complex is distorted.
Although atrial and ventricular rates can vary with third-degree block, they’re nearly the same with complete AV dissociation, a similar rhythm. (See Complete AV dissociation)
Serious Signs and Symptoms
Most patients with third-degree AV block experience significant symptoms, including severe fatigue, dyspnea, chest pain, light-headedness, changes in mental status, pulmonary edema, and loss of consciousness. You may note hypotension, pallor, diaphoresis, bradycardia, and a variation in the intensity of the pulse.
A few patients will be relatively free from symptoms, complaining only that they can’t tolerate exercise and that they’re often tired for no apparent reason. The severity of symptoms depends to a great extent on the resulting ventricular rate.
How You Intervene
If cardiac output isn’t adequate or the patient’s condition seems to be deteriorating, therapy aims to improve the ventricular rate. Atropine may be given, or a temporary pacemaker may be used to restore adequate cardiac output. Dopamine and epinephrine may also be indicated.
Temporary pacing may be required until the cause of the block resolves or until a permanent pacemaker can be inserted. A permanent block requires placement of a permanent pacemaker.
Bundles of Troubles
The patient with an anterior wall MI is more likely to have permanent third-degree AV block if the MI involved the bundle of His or the bundle branches than if it involved other areas of the myocardium. Those patients commonly require prompt placement of a permanent pacemaker.
An AV block in a patient with an inferior wall MI is more likely to be temporary, as a result of injury to the AV node. Placement of a permanent pacemaker is usually delayed in such cases to evaluate recovery of the conduction system.
Check It Out…
When caring for a patient with third-degree heart block, immediately assess the patient’s tolerance of the rhythm and the need for treatment to support cardiac output and relieve symptoms. Make sure the patient has a patent IV catheter. Administer oxygen therapy as ordered. Evaluate for possible correctable causes of the arrhythmia, such as medications or ischemia. Minimize the patient’s activity and maintain bed rest.