AUTHOR: Joseph S. Kass, MD, JD, FAAN



DefinitionGiant cell arteritis (GCA) is a segmental systemic granulomatous arteritis affecting medium and large arteries in individuals >50 yr. Inflammation primarily targets branches of the extracranial head and neck blood vessels (external carotids, temporal arteries, ciliary and ophthalmic arteries). The aorta and subclavian and brachial arteries can also be affected. Intracranial arteritis is rare.
SynonymsGCA
Temporal arteritis
Cranial arteritis
Horton disease
| ICD-10CM CODES | | M31.5 | Giant cell arteritis with polymyalgia rheumatica | | M31.6 | Other giant cell arteritis |
|
Epidemiology & DemographicsIncidenceApproximately 20 new cases per 100,000 persons >50 yr; peak incidence is in patients ages 60 to 80 yr.
Prevalence200 cases per 100,000 persons; it is the most common primary vasculitis; female:male predominance of twofold to fourfold; more common in Caucasians.
Physical Findings & Clinical PresentationGCA can present with the following clinical manifestations:
- Headache, often associated with marked scalp tenderness-noticed while brushing hair (hair comb allodynia)
- Constitutional symptoms (fever, weight loss, anorexia, fatigue)
- Polymyalgia rheumatica (aching and stiffness of the trunk and proximal muscle groups)
- Visual disturbances (transient or permanent monocular or binocular visual loss)
- Intermittent claudication of jaw and tongue on mastication that is especially prominent when solid food such as steak is chewed
- Table E1 describes atypical manifestations of GCA
TABLE E1 Atypical Manifestations of Giant Cell Arteritis
- Fever of unknown origin
- Respiratory symptoms (especially cough)
- Otolaryngeal manifestations
- Glossitis
- Lingual infarction
- Throat pain
- Hearing loss
- Large artery disease
- Aortic aneurysm
- Aortic dissection
- Limb claudication
- Raynaud phenomenon
- Neurologic manifestations
- Peripheral neuropathy
- Transient ischemic attack, stroke
- Dementia
- Delirium
- Myocardial infarction
- Tumor-like lesions
- Breast mass
- Ovarian and uterine mass
- Syndrome of inappropriate antidiuretic hormone secretion
- Microangiopathic hemolytic anemia
|
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.
Important physical findings in GCA:
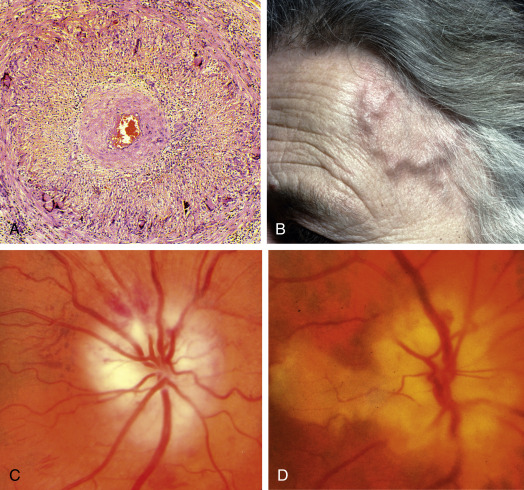
- Vascular examination: The temporal artery demonstrates tenderness, decreased pulsation, and nodularity (ropy) (Fig. E1); diminished or absent pulses in upper extremities may be seen.
Figure E1 Giant Cell ArteritisA, Histology Shows Transmural Granulomatous Inflammation, Disruption of the Internal Elastic Lamina, Proliferation of the Intima, and Gross Narrowing of the Lumen. B, The Superficial Temporal Artery is Pulseless, Nodular, and Thickened. C, Ischemic Optic Neuropathy. D, Ischemic Optic Neuropathy and Cilioretinal Artery Occlusion.
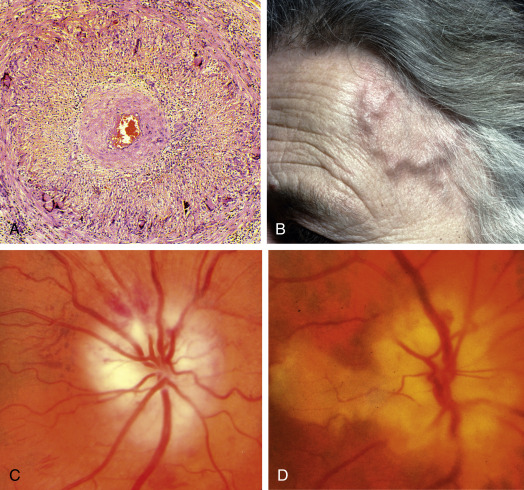
From Kanski JJ, Bowling B: Clinical ophthalmology: a systematic approach, ed 7, Philadelphia, 2010, Saunders.
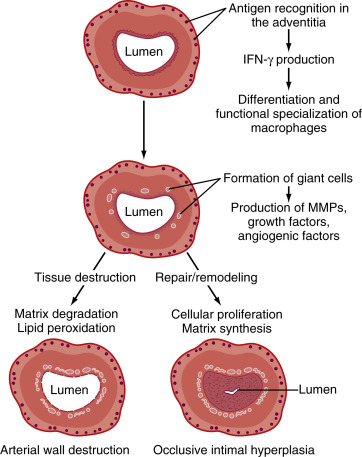
EtiologyVasculitis of unknown etiology. An association with HLA-DRB∗04 has been identified. Recent demonstration of varicella zoster virus virion, antigen, and DNA within the vessel walls of the temporal arteries on histopathologic specimens of GCA suggest an association. A proposed model for the pathogenesis of GCA is illustrated in Fig. E2.
Figure E2 Proposed Model for the Pathogenesis of Giant Cell ArteritisIfn, Interferon; Mmps, Matrix Metalloproteinases.
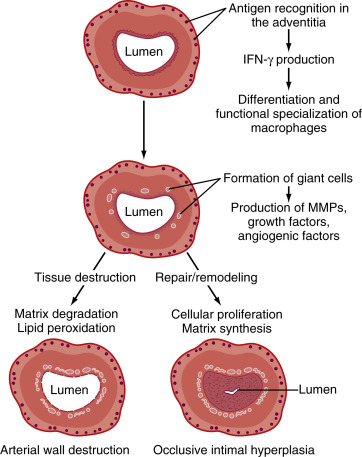
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.

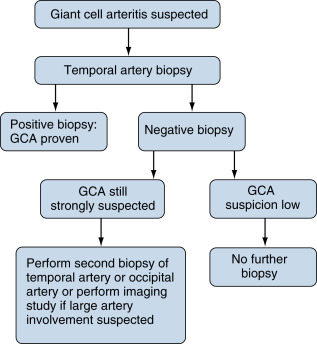
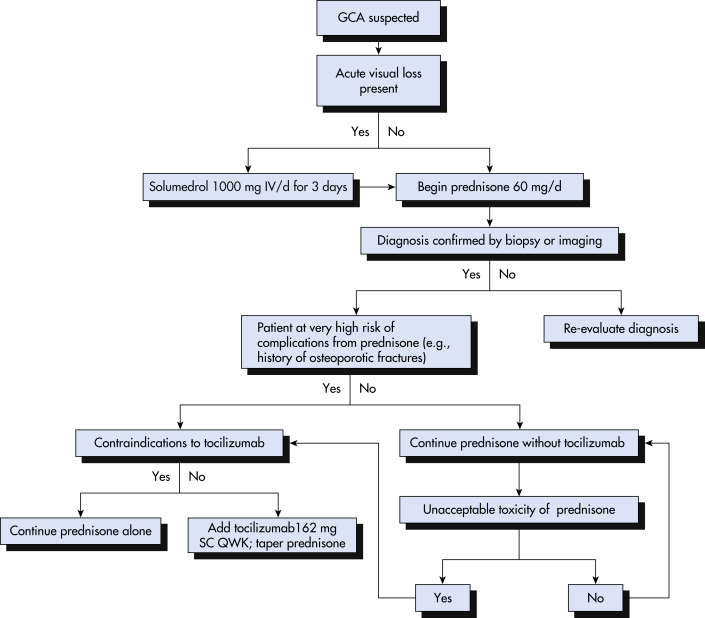
Clinical history and vascular examination remain cornerstones of diagnosis. An algorithm for diagnosing GCA is described in Fig. E3. The American College of Rheumatology has proposed classification criteria to aid in the diagnosis of GCA. Presence of three or more of these criteria in a patient with suspected vasculitis is considered suggestive of GCA:
- Age of onset of symptoms ≥50 yr
- New onset of or new type of localized headache
- Temporal artery abnormalities including tenderness or decreased pulsation
- Westergren erythrocyte sedimentation rate (ESR) elevated (typically >50 mm/h)
- Temporal artery biopsy with vasculitis and mononuclear cell infiltrate or granulomatous changes
Figure E3 Algorithm for diagnosing giant cell arteritis (GCA).

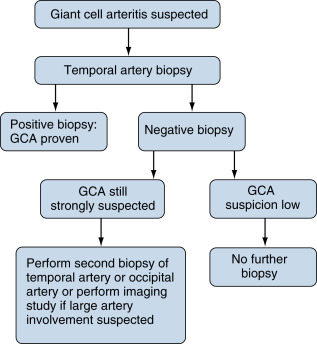
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.
Differential Diagnosis
- Polymyalgia rheumatica (Table E2)
- Other vasculitis syndromes
- Nonarteritic anterior ischemic optic neuropathy (NAION)
- Pituitary apoplexy
- Primary amyloidosis
- Transient ischemic attack, stroke
- Infections
- Occult neoplasm, multiple myeloma
TABLE E2 Differential Diagnosis of Giant Cell Arteritis and Polymyalgia Rheumatica
| Disease Type | Specific Entities |
|---|
| Giant Cell Arteritis |
| Occult infections | Tuberculosis, bacterial endocarditis, human immunodeficiency virus |
| Malignancy | Lymphoma and multiple myeloma |
| Systemic amyloidosis | - |
| Other forms of vasculitis | Takayasu arteritis, antineutrophil cytoplasmic antibody-associated vasculitis, polyarteritis nodosa, primary angiitis of the CNS |
| Other vascular disorders causing anterior ischemic optic neuropathy |
| Polymyalgia Rheumatica |
| Early rheumatoid arthritis | - |
| Polymyositis | - |
| Chronic infections | Bacterial endocarditis |
| Fibromyalgia | - |
| Complication of medication | Statins |
| Endocrine disorders | Hypothyroidism |
| Remitting, seronegative synovitis with pitting edema | - |
CNS, Central nervous system.
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia 2021, Elsevier.
Laboratory Tests
- ESR elevated, although up to 22% of patients with GCA have normal ESR before treatment.
- C-reactive protein (CRP) is typically included in laboratory investigation; it may have greater sensitivity than ESR. CRP typically rises before the ESR.
- Mild to moderate normochromic normocytic anemia, elevated platelet count.
- Temporal artery biopsy: A unilateral biopsy specimen can be examined immediately by frozen section. If the frozen section is negative for GCA, the contralateral temporal biopsy can be biopsied to increase diagnostic yield.1 Unilateral biopsy only misses the diagnosis in 5% of cases.1a
Imaging StudiesImaging studies do not play a major role in diagnosing GCA and are rarely indicated:
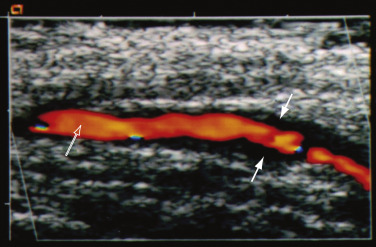
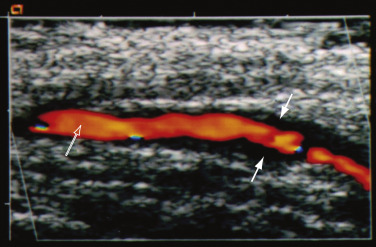
- Color duplex ultrasonography (CDUS) of temporal artery produces three characteristic features-periluminal “halo” over the temporal artery involved (Fig. E4), segmental arterial stenosis, and arterial luminal occlusion in severe cases. CDUS of the temporal artery has 40% to 75% sensitivity and 79% to 83% specificity for diagnosis of GCA. Clinical utility is not superior to clinical examination with biopsy.
- Contrasted MRI of temporal artery may be performed in patients with contraindications to surgical biopsy of the superficial temporal artery if treatment with steroids has not been initiated. MRI has a 78.4% sensitivity and 90.4% specificity in detecting temporal artery involvement in patients with a clinical diagnosis of GCA.
- Angiography of the arms is indicated in patients with peripheral vascular insufficiency.
- Fluorine-18-fluorodeoxyglucose (18F-FDG) PET/computed tomography (18F-FDG PET/CT) imaging may be used to detect large-vessel inflammation in GCA. Sensitivity is 64% in the maxillary or temporal arteries and increases to 82% if vertebral arteries and increases specificity is 100%.
Figure E4 Color Duplex Ultrasound Examination of a Swollen, Tender Temporal Artery in a Patient with Giant Cell ArteritisThe Variably Thickened Artery Wall is Visible as a Clear “halo” (Solid Arrows) around the Lumen in the Center (Open Arrow).
Courtesy Dr. Gene Hunder. In Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.