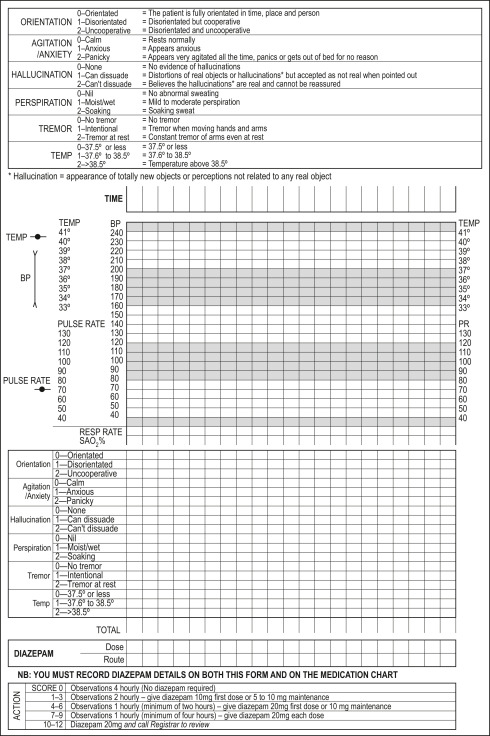
Nausea and Vomiting (0-7)0, none; 1, mild nausea with no vomiting; 4, intermittent nausea; 7, constant nausea, frequent dry heaves and vomiting Tremor (0-7)0, no tremor; 1, not visible, but can be felt fingertip to fingertip; 4, moderate, with patient’s arms extended; 7, severe, even with arms not extended Paroxysmal Sweats (0-7)0, no sweats; 1, barely perceptible sweating, palms moist; 4, beads of sweat obvious on forehead; 7, drenching sweats Anxiety (0-7)0, no anxiety, patient at ease; 1, mildly anxious; 4, moderately anxious or guarded, so anxiety is inferred; 7, equivalent to acute panic states seen in severe delirium or acute schizophrenic reactions Agitation (0-7)0, normal activity; 1, somewhat more than normal activity; 4, moderately fidgety and restless; 7, pacing back and forth during, or constantly thrashing about Tactile Disturbances (0-7)Ask, “Have you experienced any itching, pins and needles sensation, burning or numbness, or a feeling of bugs crawling on or under your skin?” 0, none; 1, very mild itching, pins and needles, burning, or numbness; 2, mild itching, pins and needles, burning, or numbness; 3, moderate itching, pins and needles, burning, or numbness; 4, moderately severe tactile hallucinations; 5, severe hallucinations; 6, extremely severe hallucinations; 7, continuous hallucinations Auditory Disturbances (0-7)Ask, “Are you more aware of sounds around you? Are they harsh? Do they startle you? Do you hear anything that disturbs you or that you know isn’t there?” 0, not present; 1, very mild harshness or ability to startle; 2, mild harshness or ability to startle; 3, moderate harshness or ability to startle; 4, moderate hallucinations; 5, severe hallucinations; 6, extremely severe hallucinations; 7, continuous hallucinations Visual Disturbances (0-7)Ask, “Does the light appear to be too bright? Is its color different than normal? Does it hurt your eyes? Are you seeing anything that disturbs you?” 0, not present; 1, very mild sensitivity to light; 2, mild sensitivity; 3, moderate sensitivity; 4, moderate hallucinations; 5, severe hallucinations; 6, extremely severe hallucinations; 7, continuous hallucinations Headache (0-7)0, not present; 1, very mild; 2, mild; 3, moderate; 4, moderately severe; 5, severe; 6, very severe; 7, extremely severe Orientation and Clouding of Sensorium (0-4)Ask, “What day is this? Where are you? Who am I?” 0, oriented; 1, cannot do serial additions or is uncertain about date; 2, disoriented to date by no more than 2 calendar days; 3, disoriented to date by more than 2 calendar days; 4, disoriented to place and/or person Total Score
- 0-9: Absent or minimal withdrawal
- 10-19: Mild to moderate withdrawal
- More than 20: Severe withdrawal
|