AUTHOR: Fred F. Ferri, MD
Hypopituitarism (from the Latin pituita, meaning “phlegm”) is the deficiency of one or more of the hormones of the anterior or posterior pituitary gland resulting from diseases of the hypothalamus or pituitary gland. Panhypopituitarism indicates the loss of all the pituitary hormones but is often used in clinical practice to describe patients deficient in growth hormone (GH), gonadotropins, corticotropin, or thyrotropin in whom posterior pituitary function remains intact.
| ||||||||||||||||
Symptoms depend on type of onset, number and severity of hormone deficiencies, their target organs, and age of onset (Table 1). Physiologic regulators of pituitary hormone secretion are summarized in Table 2.
- Mass effect of a pituitary tumor can cause headaches and visual disturbances (typically as bitemporal hemianopsia).
- Rhinorrhea.
- Corticotropin deficiency:
- Fatigue and weakness, no appetite, abdominal pain, nausea, vomiting, failure to thrive in children, and hyponatremia. If the onset is abrupt, hypotension and shock.
- Thyrotropin deficiency:
- Fatigue and weakness, weight gain, cold intolerance, anemia, constipation
- Bradycardia, hung-up reflexes, pretibial edema, change in voice, and hair loss
- Gonadotropin deficiency:
- Loss of libido, erectile dysfunction, amenorrhea, hot flashes, dyspareunia, infertility, gynecomastia, decreased muscle mass, and anemia
- GH deficiency:
- Growth retardation in children
- Easy fatigue, hypoglycemia
- Lean mass is reduced and fat mass is increased, leading to obesity
- Decreased bone mineral density, increased low-density lipoprotein cholesterol, obesity, increased inflammatory cardiovascular markers (interleukin-6 and C-reactive protein)
- Hyperprolactinemia:
- Galactorrhea, hypogonadism, inability to lactate after delivery
- Posterior pituitary (vasopressin; antidiuretic hormone [ADH] deficiency): Diabetes insipidus with polyuria, polydipsia, nocturia, hypotension, and dehydration
TABLE 1 Clinical Effects of Pituitary Hormone Deficiencies
| In panhypopituitarism, all are combined, although diabetes insipidus (ADH deficiency) is often absent | ||
|---|---|---|
| Hormone | Context | Symptoms and Signs |
| ACTH | Acute | Fatigue, weakness, hypotension, weakness, vomiting |
| Chronic | As in Addison disease, except lack of pigmentation, electrolyte disturbance and hypovolemia Hypoglycemia, weight loss | |
| TSH | Children | Growth retardation |
| Adults | As for primary hypothyroidism, thyroid atrophy | |
| GH | Children | Growth retardation, increased adiposity |
| Adults | ↓Exercise capacity, ↓ lean mass, ↑ fat mass, ↑ cardiovascular risk | |
| Gonadotropins | Children | Failure of sexual maturation, lack of pubertal growth spurt |
| Men | As for primary hypogonadism, testicular atrophy, infertility | |
| Women | Secondary amenorrhea, infertility, osteoporosis | |
| Prolactin | Women | Failure of lactation |
| Vasopressin (ADH) | Polyuria, dilute urine, thirst, nocturia, hypernatremia | |
ACTH, Adrenocorticotropic hormone; ADH, antidiuretic hormone; GH, growth hormone, TSH, thyroid-stimulating hormone.
From Talley NJ et al: Essentials of internal medicine, ed 4, Chatswood, NSW, 2021, Elsevier Australia.
TABLE E2 Physiologic Regulators of Pituitary Hormone Secretion
| Hormone | Stimulator | Inhibitor |
|---|---|---|
| Adrenocorticotropic hormone (ACTH) | Corticotrophin-releasing hormone (CRH) | |
| Thyroid-stimulating hormone (TSH) | Thyrotropin-releasing hormone (TRH) | |
| Luteinizing hormone/follicle-stimulating hormone [LH/FSH) | Gonadotropin-releasing hormone (GnRH) | Prolactin |
| Growth hormone (GH) | Growth-hormone-releasing hormone (GHRH) Ghrelin | Somatostatin |
| Prolactin (PRL) | TRH | Dopamine |
It can be congenital or acquired:
- Congenital: Mutations in transcription factors produce multiple hormonal deficiencies. Mutations in genes produce single hormonal deficiency.
- Acquired (Table 3): The result of destruction of pituitary cells caused by:
- Pituitary apoplexy: Hemorrhage or infarction of the pituitary gland. Predisposing factors include diabetes mellitus, anticoagulation therapy, head trauma, and radiation therapy. Sheehan syndrome: Postpartum necrosis, a rare complication after pregnancy.
- Infiltrative disease, including sarcoidosis, hemochromatosis, histiocytosis X, Wegener granulomatosis, lymphocytic hypophysitis, and infection of the pituitary (tuberculosis, mycosis, syphilis).
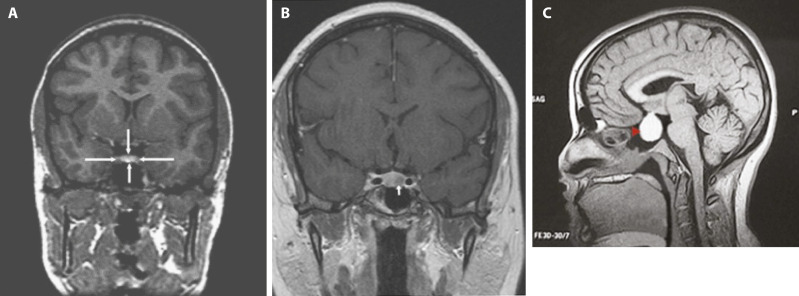
- Primary empty sella syndrome: Flattening of the pituitary gland caused by extension of the subarachnoid space and filling of cerebrospinal fluid into the sella turcica.
- Pituitary tumors: Classified by size (microadenomas, <10 mm; macroadenomas, >10 mm) and function. Prolactin-secreting tumors and nonfunctioning tumors account for the majority of pituitary adenomas.
- Suprasellar tumors: Craniopharyngiomas are the most common.
TABLE 3 Causes of Acquired Pituitary Insufficiency
| Traumatic | |||
| Infiltrative/Inflammatory | |||
| Infections | |||
| Vascular | |||
| Neoplastic | |||
| Functional | |||
GnRH, Gonadotropin-releasing hormone.
Modified from Kaiser U, Ho KKY: Pituitary physiology and diagnostic evaluation. In Melmed S et al (eds): Williams textbook of endocrinology, ed 13, Philadelphia, 2016, Elsevier; and Kliegman RM: Nelson textbook of pediatrics, ed 21, Philadelphia, 2020, Elsevier, Table 8.5, p. 193.