AUTHORS: Philip A. Chan, MD, MS, and Glenn G. Fort, MD, MPH
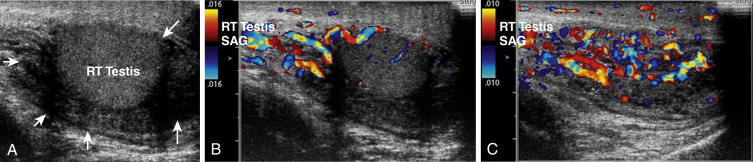
- Epididymitis is an inflammatory reaction of the epididymis caused by either an infectious agent or local trauma. In most cases of acute epididymitis, the testis is also involved (orchitis).
- Epididymitis is considered chronic if lasting ≥6 wk. Chronic epididymitis has been subcategorized into inflammatory chronic epididymitis, obstructive chronic epididymitis, and chronic epididymalgia.
Nonspecific bacterial epididymitis
Sexually transmitted epididymitis
| ||||||||||||
- Tender swelling of the scrotum with erythema, usually unilateral testicular pain and tenderness
- Dysuria and/or urethral discharge
- Fever and signs of systemic illness (less common)
- Pain and redness on scrotal examination
- Hydrocele or even epididymo-orchitis, especially late
- Chronic draining scrotal sinuses with a “bead-like” enlargement of the vas deferens in tuberculous disease
- In young, sexually active men (<35 yr of age), the most common causes of infections are Neisseria gonorrhoeae and Chlamydia trachomatis.
- In older men (>35 yr of age) or those with underlying urologic disease:
- Acute epididymitis caused by sexually transmitted enteric organisms (e.g., E. coli) also occurs among men who are the insertive partner during anal intercourse.
- Young, prepubertal boys may present with epididymitis caused by coliform bacteria; almost always a complication of underlying urologic disease such as reflux.
- In AIDS patients, cytomegalovirus (CMV) and Salmonella epididymitis have been described. CMV may have a negative urine culture. Toxoplasmosis and Cryptococcus should also be considered as a cause of epididymitis in AIDS patients.
- Chronic infectious epididymitis is most frequently seen in conditions associated with granulomatous reaction; TB is the most common granulomatous disease affecting the epididymis.