AUTHOR: Fred F. Ferri, MD
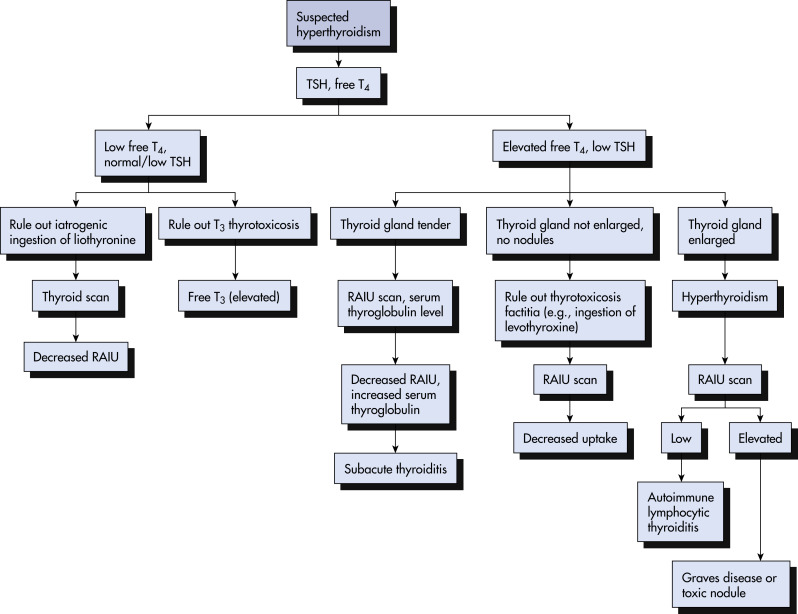
Hyperthyroidism is a hypermetabolic state resulting from excess thyroid hormone. Thyrotoxicosis is a general term for excess circulating and tissue hormone levels.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- Patients with hyperthyroidism generally present with tachycardia, tremor, hyperreflexia, anxiety, irritability, emotional lability, panic attacks, heat intolerance, sweating, increased appetite, diarrhea, weight loss, menstrual dysfunction (oligomenorrhea, amenorrhea). Presentation may be different in elderly patients (see the following).
- Patients with Graves disease may present with exophthalmos, lid retraction, and lid lag (Graves ophthalmopathy). The following signs and symptoms of ophthalmopathy may be present: Blurring of vision, photophobia, increased lacrimation, double vision, and deep orbital pressure. Clubbing of fingers associated with periosteal new bone formation in other skeletal areas (Graves acropachy) and pretibial myxedema may also be noted.
- Clinical signs of hyperthyroidism in the elderly may be masked by manifestations of coexisting disease (e.g., new-onset atrial fibrillation, exacerbation of congestive heart failure).
TABLE 1 Causes of Hyperthyroidism
| I. Excessive TSH-Receptor Stimulation | |||
| Graves disease (TRAb) Pregnancy-associated transient hyperthyroidism (hCG) Trophoblastic disease (hCG) Familial gestational hyperthyroidism (mutant TSH receptor) TSH-producing pituitary adenoma | |||
| II. Autonomous Thyroid Hormone Secretion | |||
| Multinodular toxic goiter (somatic mutations) Solitary toxic thyroid adenoma (somatic mutation) Congenital activating TSH-receptor mutation (genomic mutation) | |||
| III. Destruction of Follicles With Release of Hormone | |||
| Subacute de Quervain thyroiditis (virus infection) Painless thyroiditis/postpartum thyroiditis (hashitoxicosis-autoimmune) Acute thyroiditis (bacterial infection) Drug-induced thyroiditis (amiodarone, interferon-γ) | |||
| IV. Extrathyroidal Sources of Thyroid Hormone | |||
| Iatrogenic overreplacement with thyroid hormone Excessive self-administered thyroid medication Food and supplements containing excessive thyroid hormone Functional thyroid cancer metastases Struma ovarii |
hCG, Human chorionic gonadotropin; TRAb, thyrotropin-receptor antibodies; TSH, thyroid-stimulating hormone (thyrotropin).
From Melmed S et al: Williams textbook of endocrinology, ed 14, St Louis, 2019, Elsevier.
- Graves disease (diffuse toxic goiter): 80% to 90% of all cases of hyperthyroidism
- Toxic multinodular goiter (Plummer disease)
- Toxic adenoma
- Iatrogenic and factitious
- Transient hyperthyroidism (subacute thyroiditis, Hashimoto thyroiditis)
- Rare causes: Hypersecretion of thyroid-stimulating hormone (TSH) (e.g., pituitary neoplasms), struma ovarii, ingestion of large amount of iodine in a patient with preexisting thyroid hyperplasia or adenoma (Jod-Basedow phenomenon), hydatidiform mole, carcinoma of thyroid, amiodarone therapy