AUTHOR: Fred F. Ferri, MD
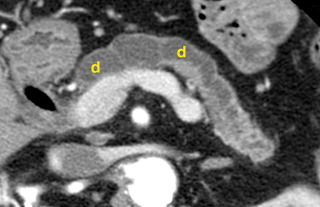
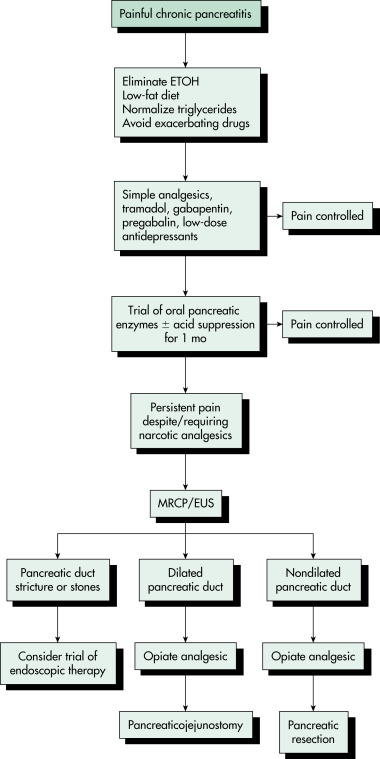
Chronic pancreatitis is a recurrent or persistent inflammatory process of the pancreas characterized by chronic pain and by pancreatic exocrine and/or endocrine insufficiency. It is classified anatomically as either large-duct disease or small-duct (minimal change) disease.
| ||||||||||||
- Chronic pancreatitis occurs in approximately 5 to 10 per 100,000 persons in industrialized countries and is usually associated with alcohol use, smoking, and certain gene mutations. It typically begins with recurrent painful bouts of pancreatitis followed by the insidious onset of chronic debilitating pain during the next 3 to 5 years after an initial episode.1
- Average age at diagnosis is 35 to 55 yr; male:female ratio is 5:1.
- Annual incidence in the U.S. is 5 to 8 per 100,000 adults.
- Prevalence in the U.S. is 42 to 73 per 100,000 adults.2
- Chronic alcoholism (most common cause)
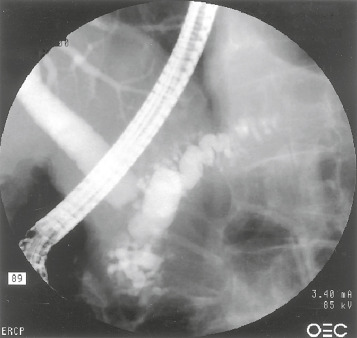
- Obstruction (ampullary stenosis, tumor, trauma [with pancreatic duct stricture], pancreas divisum, annular pancreas)
- Tobacco
- Recurrent pancreatitis
- Vascular disease/ischemia
- Hypertriglyceridemia
- Chronic kidney disease
- Hereditary pancreatitis
- Severe malnutrition
- Idiopathic
- Untreated hyperparathyroidism (hypercalcemia)
- Mutations of the cystic fibrosis transmembrane conductance regulator (CFTR) gene and the TF genotype
- Other genetic mutations (cationic trypsinogen gene, chymotrypsinogen C gene, calcium-sensing receptor gene, claudin-2 gene, serine protease inhibitor, Kazal type 1 gene)
- Autoimmune pancreatitis (AIP): (5% of chronic pancreatitis cases): Presents clinically with jaundice (63% of patients) and abdominal pain (35%). Computed tomography (CT) may reveal diffusely enlarged pancreas, enhanced peripheral rim of hypoattenuation “halo,” and low-attenuation mass in head of pancreas. Laboratory values reveal elevated serum immunoglobulin (Ig) G4, elevated serum Ig or gamma-globulin level, presence of antilactoferrin antibody (ALA), anticarbonic anhydrase (ACA) II level, antismooth-muscle antibody (ASMA), or antinuclear antibody (ANA)
- Sclerosing pancreatitis: A form of chronic pancreatitis characterized by infrequent attacks of abdominal pain, irregular narrowing of the pancreatic duct, and swelling of the pancreatic parenchyma; patients have high levels of serum immunoglobulins (IgG4); chronic sclerosing pancreatitis is also known as autoimmune pancreatitis