AUTHOR: Fred F. Ferri, MD
- Primary hyperlipoproteinemia is a group of genetic disorders of the lipid transport proteins in the blood that manifests as abnormally elevated levels of cholesterol, triglycerides, or both in the serum of affected patients.
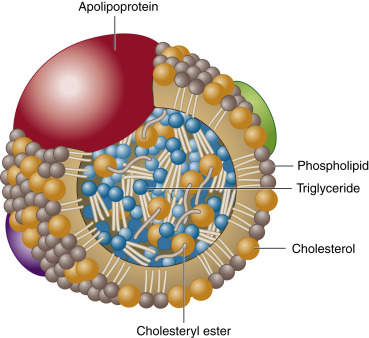
- Usually defined as total cholesterol, low-density lipoprotein (LDL), triglycerides, or lipoprotein A levels above 90th percentile or high-density lipoprotein (HDL) or apo A-1 levels below the 10th percentile for the general population. Fig. E1 illustrates the structure of lipoproteins. Plasma lipoprotein composition is described in Table E1.
Figure E1 Structure of lipoproteins.
Phospholipids are oriented with their polar group toward the aqueous environment of plasma. Free cholesterol is inserted within the phospholipid layer. The core of the lipoprotein is made up of cholesteryl esters and triglycerides. Apolipoproteins are involved in the secretion of the lipoprotein, provide structural integrity, and act as cofactors for enzymes or as ligands for various receptors.
From Bonow RO et al: Heart disease, ed 9, Philadelphia, 2012, Saunders.
TABLE E1 Plasma Lipoprotein Composition
| Component | Origin | Density (g/ml) | Size (nm) | Protein (%) | Cholesterol in Plasma (mmol/L)† | Triglyceride in Fasting Plasma (mmol/L)‡ | Apoprotein | |
|---|---|---|---|---|---|---|---|---|
| Major | Other | |||||||
| Chylomicron∗ | Intestine | <0.95 | 100-1000 | 1-2 | 0.0 | 0.0 | B48 | A-I, Cs |
| Chylomicron remnants∗ | Chylomicron metabolism | 0.95-1.006 | 30-80 | 3-5 | 0.0 | 0.0 | B48, E | A-I, A-IV, Cs |
| VLDL | Liver | <1.006 | 40-50 | 10 | 0.1-0.4 | 0.2-1.2 | B100 | AI, Cs |
| IDL | VLDL | 1.006-1.019 | 25-30 | 18 | 0.1-0.3 | 0.1-0.3 | B100, E | |
| LDL | IDL | 1.019-1.063 | 20-25 | 25 | 1.5-3.5 | 0.2-0.4 | B100 | |
| HDL | Liver, intestine | 1.063-1.210 | 6-10 | 40-55 | 0.9-1.6 | 0.1-0.2 | A-I, A-II | A-IV |
| Lipoprotein(a) | Liver | 1.051-1.082 | 25 | 30-50 | B100, (a) | |||
HDL, High-density lipoprotein; IDL, intermediate-density lipoprotein; LDL, low-density lipoprotein; VLDL, very low-density lipoprotein.
∗In the fasted state, serum (or plasma) should not contain chylomicrons or their remnants.
† In mmol/L. For mg/dl, multiply by 38.67.
‡ In mmol/L. For mg/dl, multiply by 88.5.
From Bonow RO et al: Heart disease, ed 9, Philadelphia, 2012, Saunders.
| ||||||||||||||||||||||||
The most common types are lipoprotein A excess, hypertriglyceridemia, and combined hyperlipidemia.
- Incidence of heterozygous familial hypercholesterolemia: 1:500
- Incidence of homozygous familial hypercholesterolemia: 1:1 million
- Familial hypercholesterolemia: Autosomal dominant disorder
- Familial combined hyperlipidemia: Possibly an autosomal dominant disorder
- Multifactorial predilection: Apparent in majority of affected individuals
- Familial lipoprotein lipase deficiency: Autosomal recessive, resulting in an elevation in the plasma chylomicrons and triglycerides
- Familial apoprotein CII deficiency: Autosomal recessive, resulting in increased serum chylomicrons, very low-density lipoprotein (VLDL), and hypertriglyceridemia
- Familial type 3 hyperlipoproteinemia: Single-gene defect requiring contributory factors to manifest
- Familial hypercholesterolemia: Autosomal dominant defect of the LDL receptor, resulting in an elevated serum cholesterol level and normal triglycerides. HoFH is the most severe form of the disease. LDL levels can reach over 500 mg/dl and can cause death in childhood
- Familial hypertriglyceridemia: Common, autosomal dominant defect resulting in elevated VLDL and triglycerides
- Multiple lipoprotein-type hyperlipidemia: Autosomal dominant, manifesting as isolated hypercholesterolemia, isolated hypertriglyceridemia, or hyperlipidemia
- Polygenic hypercholesterolemia: Multifactorial
- Polygenic hyperalphalipoproteinemia: Autosomal dominant or polygenic, causing an elevated HDL
- A classification of lipoprotein disorders and their clinical findings and management are summarized in Table 2
TABLE 2 Disorders of Lipids: Clinical Findings and Management
| Disorder | Xanthomas | Cardiovascular | Gastrointestinal | Neurologic | Ophthalmologic | Other Findings | Management |
|---|---|---|---|---|---|---|---|
| Type I | Eruptive, tendinous, xanthelasmas | None | Acute abdomen, hepatosplenomegaly, pancreatitis | None | Lipemia retinalis, retinal vein occlusion | Diabetes, lipemic plasma | Diet, plasmapheresis |
| Type II | Planar, especially intertriginous, tendinous, tuberous | Generalized atherosclerosis | None | None | Arcus cornea | None | Type IIa: Bile acid sequestrants, statins, niacin, fish oil Type IIb: Statins, niacin, fibrate |
| Type III | Planar, especially palmar, tuberous | Atherosclerosis | None | None | None | Abnormal glucose tolerance, hyperuricemia | Statins, fibrate |
| Type IV | Eruptive, tuberous | Atherosclerosis | Acute abdomen, hepatosplenomegaly, pancreatitis | None | Lipemia retinalis | Obesity | Statins, fibrate, niacin |
| Type V | Eruptive, tuberous | Atherosclerosis | Acute abdomen, hepatosplenomegaly, pancreatitis | None | Lipemia retinalis | Obesity, hyperinsulinemia | Niacin, fibrate |
| Tangier | Macular rash, foam cells in biopsies | Atherosclerosis | Acute abdomen, hepatosplenomegaly | Peripheral neuropathy | Corneal infiltration | Enlarged orange tonsils, lymphadenopathy | |
| Apolipoprotein A-I and C-III deficiency | Planar and tendon xanthomas, foam cells in biopsies | Atherosclerosis | Normal | Normal | Corneal clouding | None | |
| HDL deficiency with planar xanthomas | Planar xanthomas, foam cells in biopsies | Atherosclerosis | Hepatomegaly | Normal | Corneal opacity | None |
HDL, High-density lipoprotein.
From Paller AS, Mancini AJ: Hurwitz clinical pediatric dermatology: a textbook of skin disorders of childhood and adolescence, ed 5, 2016, Elsevier.
- Familial lipoprotein lipase deficiency: Recurrent bouts of abdominal pain in infancy, eruptive xanthomas, hepatomegaly, splenomegaly, lipemia retinalis
- Familial apoprotein CII deficiency: Occasional eruptive xanthomas
- Familial type 3 hyperlipoproteinemia: Xanthoma striata palmaris or tuberoeruptive xanthomas, xanthelasmas, arterial bruits at a young age, gangrene of the lower extremities at a young age
- Familial hypercholesterolemia: Tendon xanthomas, arcus corneae, xanthelasma
- Familial hypertriglyceridemia: Associated obesity; eruptive xanthomas (Fig. E2) can develop with exacerbations