AUTHOR: Kausik Umanath, MD, MS, FACP FASN
Renal artery stenosis (RAS) is progressive narrowing of the renal artery, which is most commonly due to atherosclerosis or fibromuscular dysplasia (FMD). RAS is an important, potentially reversible cause of hypertension, ischemic nephropathy, and destabilizing cardiac syndromes. RAS increases the risk of renal artery occlusion via progressive stenosis.
| ||||||||||||||||||||
- Atherosclerotic renal artery stenosis:
- Atherosclerotic renal artery stenosis (ARAS) accounts for ∼90% of cases. The true prevalence of ARAS is unknown.1
- General population autopsy studies: 10% to 27% over 50 yr; hypertensive patients, 0.2% to 5%.
- In a general population older than 65 yr, the prevalence is 6.8% by Doppler ultrasound (5.5% of women, 9.1% of men; 6.7% African Americans, and 6.9% White). Bilateral disease was present in 12% of affected individuals.
- In patients with malignant hypertension, the prevalence is 43% in White patients and 7% in African American patients. In patients with mild hypertension, the prevalence is <1%.
- In patients with peripheral artery disease, the prevalence is 22% to 59%.
- Fibromuscular dysplasia:
- FMD accounts for ∼10% of chronic RAS and is typically encountered in women (90%). FMD was previously thought to be a disease of the young and healthy, with few risk factors. Recent data suggest that the average age of onset of hypertension is 43 yr. Bilateral renal artery involvement is seen in 25% to 35% of cases.2
- Atherosclerotic renal artery stenosis (ARAS) accounts for ∼90% of cases. The true prevalence of ARAS is unknown.1
- RAS should be considered in any White female patients <30 yr with hypertension not attributed to any other cause, any patients >50 yr with new-onset refractory hypertension, or patients with stable hypertension that has abruptly and/or significantly worsened.
- RAS most often presents as a clinically asymptomatic finding. Manifestations can include renovascular hypertension, ischemic nephropathy, or flash pulmonary edema.
- Flash pulmonary edema in the absence of cardiac disease most often indicates severe bilateral RAS.
- Renovascular hypertension should be considered in individuals with resistant hypertension (lack of blood pressure control on a medication regimen that includes 3 maximally dosed medications, one of which is a diuretic).
- Ischemic nephropathy should be considered if kidney function is rapidly deteriorating or kidney sizes are decreasing on serial imaging, particularly with bilateral disease.
- Acute elevations of serum creatinine (>30%) after starting ACE inhibitors or angiotensin receptor blockers (ARBs) may be seen in bilateral disease.
- A bruit heard in either upper quadrant on abdominal auscultation may suggest RAS. Patients with ARAS will often have bruits heard in other vascular beds.
- Atherosclerosis: ARAS has similar risk factors to atherosclerosis in other vascular beds, including family history, smoking, diabetes, hypertension, and hyperlipidemia. ARAS most often involves the ostium and proximal third of the main renal artery.
- FMD (Figs. 1 and 2): Etiology is unknown. Classified into three categories based on the affected layer of arterial wall: Medial (>90%), intimal (<10%), and adventitial (<1%). FMD typically involves the distal main renal artery and intrarenal branches.
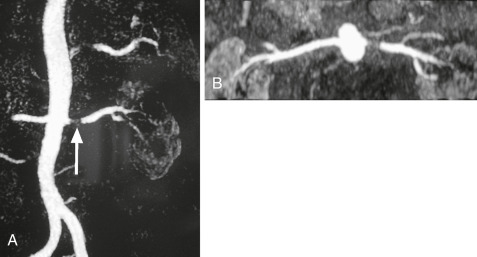
Figure 1 Magnetic resonance angiogram.
A, Coronal maximum intensity projection (MIP) of a patient with significant left renal artery stenosis (white arrow). B, Axial MIP of the same patient.
From Adam A et al: Grainger & Allison’s diagnostic radiology, ed 5, 2007, Churchill Livingstone; and Grant LA: Grainger & Allison’s diagnostic radiology essentials, ed 2, 2019, Philadelphia, Elsevier.
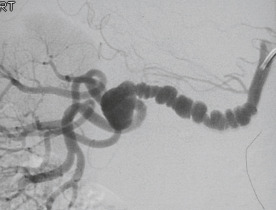
Figure 2 Fibromuscular dysplasia.
On a selective right anterior oblique (RAO) digital subtraction angiogram, the characteristic saccular dilations and weblike stenoses are clearly evident.
From Adam A et al: Grainger & Allison’s diagnostic radiology, ed 5, 2007, Churchill Livingstone; and Grant LA: Grainger & Allison’s diagnostic radiology essentials, ed 2, 2019, Philadelphia, Elsevier.
- Pathogenesis of FMD is unknown. FMD involves abnormal constrictions and dilations of the renal artery leading to a typical “string of beads” appearance on angiography.
- The pathogenesis of atherosclerotic RAS is similar to that of atherosclerosis in other vascular beds.
- The pathogenesis of renovascular hypertension is related to the neurohormonal cascade resulting from renal ischemia. Renal hypoperfusion or ischemia secondary to arterial stenosis produces an increase in plasma renin and secondary elevations of angiotensin II, with consequent vasoconstriction, aldosterone elevation, sodium retention, and renal potassium wasting. Hypertension results and can be self-sustaining, even in the case of unilateral RAS due to hypertensive damage of the contralateral kidney3.
- The pathogenesis of ischemic nephropathy is due to the activation of numerous mechanisms of tissue injury resulting in progressive renal parenchymal loss and fibrosis.
- “Flash” or sudden-onset pulmonary edema, a manifestation usually seen in bilateral ARAS, results from sodium and water retention and upregulation of the sympathetic nervous system2.
- RAS caused by FMD rarely causes renal artery occlusion or ischemic nephropathy.
- ARAS rarely progresses to total occlusion. One study of serial ultrasounds of patients with RAS demonstrated that only 5% of those with >60% stenosis progressed to total occlusion in 1 yr, and an additional 11% progressed to total occlusion by 2 yr.