AUTHOR: Fred F. Ferri, MD
| ||||||||||||||||||||||||||||||||||||||||
- Hypothyroid patients generally present with the following signs and symptoms: Fatigue, lethargy, weakness, constipation, weight gain, cold intolerance, muscle weakness, slow speech, slow cerebration with poor memory
- Skin: Dry, coarse, thick, cool, sallow (yellow color caused by carotenemia); nonpitting edema in skin of eyelids and hands (myxedema) secondary to infiltration of subcutaneous tissues by a hydrophilic mucopolysaccharide substance (Fig. E1, A and B)
- Hair: Brittle and coarse; loss of outer third of eyebrows
- Face: Dulled expression, thickened tongue, thick and slow-moving lips
- Thyroid gland: May or may not be palpable (depending on the cause of the hypothyroidism)
- Heart sounds: Distant, possible pericardial effusion
- Pulse: Bradycardia
- Neurologic: Delayed relaxation phase of the deep tendon reflexes, cerebellar ataxia, hearing impairment, poor memory, peripheral neuropathies with paresthesia
- Musculoskeletal: Carpal tunnel syndrome, muscular stiffness, weakness
Notice the Dry Skin and Sallow Complexion; Absence of Scleral Pigmentation Differentiates the Carotenemia from Jaundice. Both Individuals Demonstrate Periorbital Myxedema. The Patient in B Illustrates the Loss of the Lateral Aspect of the Eyebrow, Sometimes Termed Queen Anne Sign. That Finding is Not Unusual in the Age Group that is Commonly Affected by Severe Hypothyroidism and Should Not Be Considered a Specific Sign of the Condition.
From Melmed S et al: Williams textbook of endocrinology, ed 12, Philadelphia, 2011, Saunders.
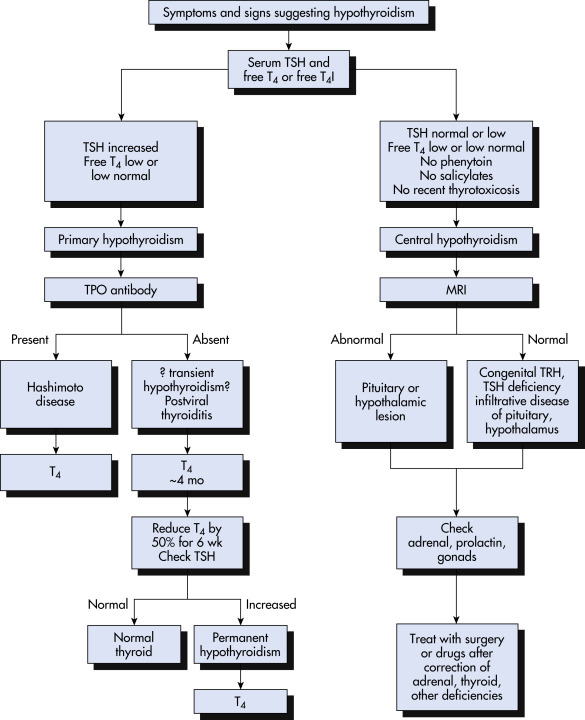
- Primary hypothyroidism (thyroid gland dysfunction): The cause of >90% of the cases of hypothyroidism
- Hashimoto thyroiditis is the most common cause of hypothyroidism after age 8 yr
- Idiopathic myxedema (nongoitrous form of Hashimoto thyroiditis)
- Previous treatment of hyperthyroidism (radioiodine therapy, subtotal thyroidectomy)
- Subacute thyroiditis
- Radiation therapy to the neck (usually for malignant disease)
- Iodine deficiency or excess
- Drugs (lithium, paraaminosalicylate, sulfonamides, phenylbutazone, amiodarone, thiourea). Box E1 summarizes medications that may cause iatrogenic hypothyroidism.
- Congenital (approximately one case per 2000 to 4000 live births)
- Prolonged treatment with iodides
- Secondary hypothyroidism: Pituitary dysfunction, postpartum necrosis, neoplasm, infiltrative disease-causing deficiency of TSH
- Tertiary hypothyroidism: Hypothalamic disease (granuloma, neoplasm, or irradiation causing deficiency of thyrotropin-releasing hormone)
- Tissue resistance to thyroid hormone: Rare
TABLE 1 Causes of Hypothyroidism
| Primary Hypothyroidism | |||
| Acquired | |||
| |||
| Congenital | |||
| |||
| Consumptive Hypothyroidism | |||
| Defects of Thyroxine to Triiodothyronine Conversion | |||
| Central Hypothyroidism | |||
| Acquired | |||
| Congenital | |||
| Resistance to Thyroid Hormone | |||
NIS, Sodium-iodide symporter; TPO, thyroid peroxidase; TSH, thyroid-stimulating hormone (thyrotropin).
From Melmed S et al: Williams textbook of endocrinology, ed 14, Philadelphia, 2019, Elsevier.
BOX E1 Medications That May Cause Iatrogenic Hypothyroidism
IV, Intravenous; T4, thyroxine; TSH, thyroid stimulating hormone.
Inhibition of Thyroid Hormone Synthesis or Secretion
|
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.