AUTHOR: Fred F. Ferri, MD




DefinitionProlactinomas are monoclonal tumors that secrete prolactin.
| ICD-10CM CODES | | D35.2 | Benign neoplasm of pituitary gland | | E22.8 | Other hyperfunction of pituitary gland |
|
Epidemiology & DemographicsIncidenceMost common pituitary tumor; nearly 30% of all pituitary adenomas secrete enough prolactin to cause hyperprolactinemia.
Predominant SexMicroadenomas are more common in women; macroadenomas are found more frequently in men.
Physical Findings & Clinical Presentation
- Men: Decreased facial and body hair, infertility, small testicles; may also have de creased libido, erectile dysfunction, and delayed puberty (caused by decreased testosterone as a result of inhibition of gonadotropin secretion).
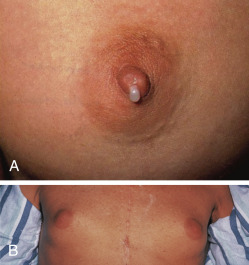
- Women: Physical examination may be normal; history may reveal amenorrhea, galactorrhea (Fig. E1), oligomenorrhea, and anovulation.
- Both sexes: Visual field defects and headache may occur depending on size of tumor and its expansion.
Figure E1 Effects of prolactinoma.
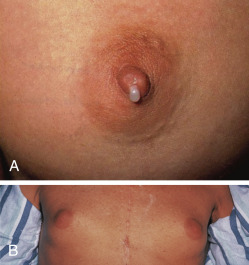
A, Galactorrhea in a female. B, Gynecomastia in a male.
A, From Bouloux PM: Clinical medicine assessment questions in color, St Louis, 1993, Wolfe; B, From Mir MA: Atlas of clinical diagnosis, Edinburgh, 2003, Saunders.
EtiologyProlactin-secreting pituitary adenomas: Microadenomas (<10 mm diameter) or macroadenomas (>10 mm diameter). No risk factors have been identified for sporadic prolactinomas. Rarely prolactinomas can be part of multiple endocrine neoplasia (MEN) type 1 syndrome.