AUTHORS: Anthony Sciscione, DO and Kathryn G. Vollum, MD
Fibrocystic breast disease (FBD), or fibrocystic breast changes (FBC), is a category of benign breast lesions that includes:
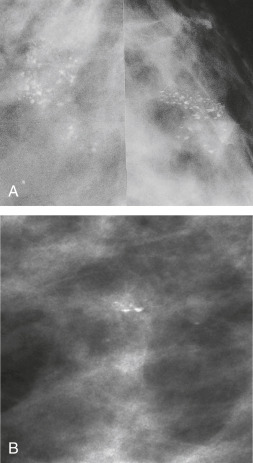
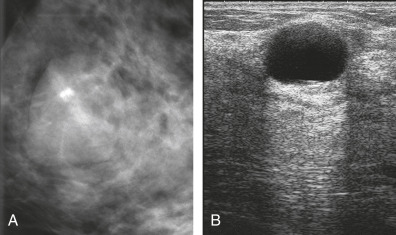
- Microcystic and macrocystic changes
- Fibrosis
- Mild and moderate hyperplasia
- Sclerosing adenosis
- Apocrine metaplasia
- Fibroadenoma
- Papilloma
- Papillomatosis
- Radial scar
Nonmalignant breast lesions can be divided into nonproliferative, proliferative without atypia, and atypical hyperplasia. Nonproliferative lesions such as simple breast cysts and galactoceles, are considered not to be at increased risk for breast cancer (RR = 1.17). Proliferative lesions, including ductal hyperplasia, intraductal papillomas, sclerosing adenosis, radial scars, and fibroadenomas, are considered markers for a small increase in risk of progressing to breast cancer (proliferation without atypia RR = 1.76, with hyperplastic atypia RR = 3.93), and patients should be counseled on risk reduction.
| ||||||||||||||||||||||||||||||||
- FBC affects 30% to 60% of reproductive-age women.
- Most commonly seen in women ages 30 to 50 yr.
- Prevalence of various benign breast changes in the postmenopausal cohort is increased by a factor of 1.7 in those receiving exogenous estrogen and progestins.