AUTHOR: Nicholas J. Lemme, MD
Systemic juvenile idiopathic arthritis (SJA) is defined as arthritis that occurs in children aged 16 yr or younger and is associated with a daily fever that persists for longer than 2 wk, a characteristic short-lived erythematous maculopapular rash, and at least one of the following associated features: lymphadenopathy, pericarditis, pleuritis, or hepatosplenomegaly.
The International League of Associations for Rheumatology (ILAR) Diagnostic Criteria for Systemic juvenile idiopathic arthritis (SJA) is summarized in Box E1. Box E2 describes the operational case definition for new-onset SJA adapted from CARRA Consensus Treatment Plans.
BOX E1 Systemic Juvenile Idiopathic Arthritis: International League of Associations for Rheumatology (ILAR) Diagnostic Criteria
Arthritis in any number of joints together with a fever of at least 2 wk duration that is documented to be daily (quotidian) for at least 3 days and is accompanied by one or more of the following:
|
From Petty RE et al: Textbook of pediatric rheumatology, ed 8, Philadelphia, 2021, Elsevier.
Systemic juvenile rheumatoid arthritis
Systemic juvenile chronic arthritis
| ||||||||
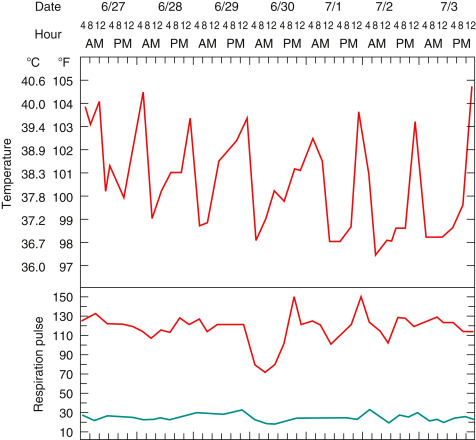
- SJA presents with a fever which typically exceeds 39° C and oscillates during a 24-h period (Fig. E1).
- Typically, the peaks in fever are observed concomitantly with a transient salmon-colored maculopapular rash (Fig. E2).
- The arthralgias observed can affect any joint, can be oligo- or polyarticular, and are usually symmetric in nature.
- Other systemic findings that can be observed are abdominal pain secondary to serositis, headaches, and pleuritis.
- The disease course is extremely variable and can include a fever and rash that last 2 to 3 wk and are followed by mild systemic symptoms vs. the onset of all the above symptoms at once.
- Macrophage activation syndrome (MAS) is a severe complication that can occur during SJA disease onset and is characterized by a persistent fever, atypical rash, coagulopathy, anemia, and hyperferritinemia.
Figure E1 Intermittent fever of systemic juvenile idiopathic arthritis in a 3-yr-old girl.
The fever spikes usually occurred daily in the late evening to early morning (quotidian pattern), returned to normal or below normal, and were accompanied by severe malaise, tachycardia, and rash.
From Petty RE et al: Textbook of pediatric rheumatology, ed 8, Philadelphia, 2021, Elsevier.
Figure E2 Typical rash of systemic juvenile idiopathic arthritis in a 3-yr-old boy.
The rash is salmon-colored, macular, and nonpruritic. Individual lesions are transient, occur in crops over the trunk and extremities, and may occur in a linear distribution (Koebner phenomenon) after minor trauma such as scratching.
From Petty RE et al: Textbook of pediatric rheumatology, ed 8, Philadelphia, 2021, Elsevier.
The etiology of SJA is currently unknown; however, there is data to suggest that interleukin-1 (IL-1) and IL-6 are primary contributors to the pathogenesis of the disease.
∗Daily fever is not required but must at some point exhibit a quotidian fever pattern.
† Swelling within a joint, or limitation in the range of joint movement with joint pain or tenderness, is observed by a physician, and is not the result of primarily mechanical disorders or other identifiable causes.
‡ Infections, malignancy, and other diagnoses that can present with similar symptoms as sJIA should be excluded before initiating treatment plans for new-onset sJIA in order to avoid unintended adverse effects of the treatment plans if used for other diagnoses.