Author: Kapil S. Meleveedu, MD
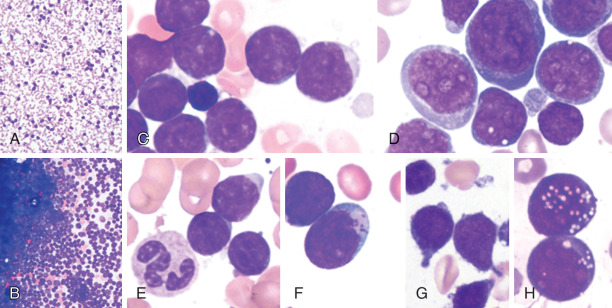
Acute lymphoblastic leukemia (ALL) is a malignancy of precursor B or T lymphocytes (lymphoblasts) characterized by uncontrolled proliferation of malignant lymphocytic cells with replacement of normal bone marrow elements and bone marrow failure. Lymphoblastic lymphoma (LBL) is diagnosed when the disease presents in extramedullary sites (most commonly as mediastinal mass in T-cell disease) and <20% of the bone marrow is involved.
| ||||||||||||||||
- ALL is primarily a disease of children, adolescents, and young adults.
- Overall incidence is 1.8/100,000 persons per year; 65% are <34 yr. It is most commonly diagnosed among people aged <20.
- Incidence varies according to race and ethnic group, being more common in Hispanics and Whites than Blacks.
- Male:female ratio is 55:45.
Expected overall 5 yr relative survival is 71% but substantially better in children and approaches 95%.
- Findings consistent with bone marrow failure and peripheral cytopenias-pallor, bruising, petechiae
- Lymphadenopathy or hepatosplenomegaly
- Fever (disease related or infectious), bone pain, weakness, weight loss, mental status changes, and neurologic findings associated with central nervous system (CNS) involvement (if present)
- T-cell LBL is usually associated with a mediastinal mass
- Table E1 summarizes the clinical presentation of acute ALL and LBL
TABLE E1 Clinical Presentation of Acute Lymphoblastic Leukemia
| Symptoms/Signs | Etiology | Management |
|---|---|---|
| Fever | Disease or infection | Always conduct fever workup and provide broad antimicrobial coverage until infectious etiology is ruled out |
| Fatigue, pallor | Anemia (ALL infiltrating bone marrow) | Packed red blood cell transfusion (slow if anemia is severe, avoid in hyperleukocytosis) |
| Petechiae, bruising, bleeding | Thrombocytopenia (ALL infiltrating bone marrow) | Transfuse with platelets |
| Pain | Leukemia infiltrating bones/joints, or expanding marrow cavity | Establish diagnosis and start chemotherapy |
| Respiratory distress/superior vena cava syndrome | Mediastinal mass | Avoid sedation in presence of tracheal compression. Establish diagnosis as soon as possible and start chemotherapy |
ALL, Acute lymphoblastic leukemia.
From Hoffman R et al: Hematology, basic principles and practice, ed 8, Philadelphia, 2023, Elsevier.
- Most cases are sporadic without established risk factors.
- Ionizing radiation exposure appears to be a risk factor.
- Down syndrome (trisomy 21) is associated with an approximately 3% risk of developing leukemia by age 30, predominantly ALL. ALL may be seen with other hereditary premalignancy syndromes (e.g., ataxia-telangiectasia).