The major classes of lung diseases include obstructive lung diseases (e.g., asthma, chronic obstructive pulmonary disease, and bronchiectasis), restrictive lung diseases (e.g., interstitial lung diseases, chest wall abnormalities, and neuromuscular diseases), and vascular abnormalities (e.g., pulmonary thromboembolism, pulmonary arterial hypertension, and pulmonary veno-occlusive disease). The respiratory system includes not only the lungs but also the chest wall, pulmonary circulation, and central nervous system. There are three key types of respiratory system physiologic disturbances that occur in varying combinations in different lung diseases: ventilatory function, pulmonary circulation, and gas exchange.
Disturbances in Ventilatory Function 
Ventilation involves the delivery of gas to the alveoli. Pulmonary function tests are used to assess ventilatory function. The classification of lung volumes, which are measured with pulmonary function testing, is shown in Fig. 128-1. Spirometry involves forced exhalation from total lung capacity (TLC) to residual volume (RV); key measurements from a spirogram are the forced expiratory volume in 1 s (FEV1) and the forced vital capacity (FVC). Expiratory flow rates may be plotted against lung volumes to yield a flow-volume curve. Plateau of the inspiratory curve on the flow-volume loop suggests extrathoracic large airway obstruction, while plateau of the expiratory curve suggests intrathoracic large airway obstruction. Other lung volumes, including TLC and RV, are measured under static conditions using either inert gas dilution or body plethysmography. Lung volumes and flow rates are typically compared with population-based normal values that adjust for the age, height, sex, and race of the pt.
There are two major patterns of abnormal ventilatory function detected by pulmonary function testing: restrictive and obstructive (Tables 128-1 and 128-2). The presence of obstruction is determined by a reduced ratio of FEV1/FVC (with abnormal often defined as <0.7), and the severity of airflow obstruction is determined by the level of reduction of FEV1. With airflow obstruction, TLC may be normal or increased, and RV is typically elevated. With severe airflow obstruction, the FVC is often also reduced.
The presence of a restrictive pattern is determined by a reduction in TLC to <80% of the pt's predicted value. When pulmonary parenchymal processes cause restriction, RV is also decreased, but the FEV1/FVC is normal. With extraparenchymal etiologies of restrictive ventilatory defects, such as neuromuscular weakness or chest wall abnormalities, the impact on RV and FEV1/FVC is more variable. Weakness of the respiratory muscles can be assessed by measuring maximal inspiratory and expiratory pressures.
Disturbances in Pulmonary Circulation 
The pulmonary vasculature normally handles the right ventricular output (~5 L/min) at a low pressure. Normal mean pulmonary artery pressure (PAP) is 15 mmHg. When cardiac output increases, pulmonary vascular resistance (PVR) normally falls, leading to only small increases in mean PAP.
Assessment of the pulmonary vasculature requires measuring pulmonary vascular pressures and cardiac output to derive PVR. PVR rises with hypoxemia (due to vasoconstriction), intraluminal thrombi (due to diminished cross-sectional area from obstruction), or destruction of small pulmonary vessels (due to scarring or loss of the alveolar walls).
All diseases of the respiratory system causing hypoxemia are capable of causing pulmonary hypertension. However, pts with prolonged hypoxemia related to chronic obstructive pulmonary disease, interstitial lung disease, chest wall disease, and obesity-hypoventilation/obstructive sleep apnea are particularly likely to develop pulmonary hypertension. When pulmonary vessels are directly affected, as with recurrent pulmonary emboli, the decrease in cross-sectional area of the pulmonary vasculature is the primary mechanism for increased PVR, rather than hypoxemia.
The primary functions of the respiratory system are to remove CO2 from blood entering the pulmonary circulation and to provide O2 to blood leaving the pulmonary circulation. Normal tidal volume is approximately 500 mL and normal respiratory rate is approximately 15 breaths/min, leading to a total minute ventilation of approximately 7.5 L/min. Because of anatomic dead space, alveolar ventilation is approximately 5 L/min. Gas exchange depends on alveolar ventilation rather than total minute ventilation.
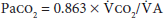
Partial pressure of CO2 in arterial blood (Paco2) is directly proportional to the amount of CO2 produced each minute ( co2) and inversely proportional to alveolar ventilation (
co2) and inversely proportional to alveolar ventilation ( A).
A).
Adequate movement of gas between alveoli and pulmonary capillaries by diffusion is required for normal gas exchange. Diffusion can be tested by measuring the diffusing capacity of the lung for a low (and safe) concentration of carbon monoxide (DLCO) during a 10-s breath hold. DLCO measurement is typically corrected for the pt's hemoglobin level. Diffusion abnormalities rarely result in arterial hypoxemia at rest but can cause hypoxemia with exercise. A restrictive ventilatory defect with reduced DLCO suggests parenchymal lung disease. The pattern of normal spirometry, normal lung volumes, and reduced DLCO is consistent with pulmonary vascular disease. Gas exchange is critically dependent on proper matching of ventilation and perfusion.
Assessment of gas exchange is commonly performed with arterial blood gases, which provide measurements of the partial pressures of O2 and CO2. The actual content of O2 in blood is determined by both Po2 and hemoglobin concentration. The alveolar-arterial O2 difference ([A-a] gradient) is reduced in diseases causing ventilation-perfusion mismatch or shunt physiology. The normal (A-a) gradient is <15 mmHg under age 30 but increases with aging. In order to calculate the (A-a) gradient, the alveolar Po2 (Paco2) must be calculated:
PAO2 = [FIO2 × (PB - PH2O)] - (Paco2/R)where FIO2 = fractional concentration of inspired O2 (0.21 while breathing room air), PB = barometric pressure (760 mmHg at sea level), PH2O = water vapor pressure (47 mmHg when air is saturated at 37°C [98.6°F]), and R = respiratory quotient (the ratio of CO2 production to O2 consumption, usually assumed to be 0.8). Severe arterial hypoxemia rarely occurs purely due to alveolar hypoventilation while breathing air at sea level. The (A-a) gradient is calculated by subtracting the measured Pao2 from the calculated PAO2.
Adequacy of CO2 removal is reflected in the partial pressure of CO2 measured in an arterial blood gas. Pulse oximetry is a valuable, widely used, and noninvasive tool to assess O2 saturation, but it provides no information about Paco2. Other limitations of pulse oximetry include relative insensitivity to oxygenation changes when Pao2 is >60 mmHg, problems with obtaining an adequate signal when cutaneous perfusion is decreased, and inability to distinguish oxyhemoglobin from other forms of hemoglobin, such as carboxyhemoglobin and methemoglobin.
Mechanisms of Abnormal Respiratory Function 
The four basic mechanisms of hypoxemia are: (1) decrease in inspired Po2, (2) alveolar hypoventilation, (3) shunt, and (4) ventilation/perfusion mismatch. Decrease in inspired Po2 (e.g., at high altitude) and hypoventilation (characterized by an increased Paco2) both lower arterial oxygenation by reducing alveolar oxygenation; thus, the (A-a) gradient is normal. Shunting (e.g., intracardiac shunt) causes hypoxemia by bypassing the alveolar capillaries. Shunting is characterized by an elevated (A-a) gradient and is relatively refractory to oxygenation improvement with supplemental O2. Ventilation/perfusion mismatch is the most common cause of hypoxemia; it is associated with an elevated (A-a) gradient, but supplemental O2 corrects the hypoxemia by raising the O2 content of blood from regions with low ventilation/perfusion ratios. An algorithm for approaching the hypoxemic pt is shown in Fig. 128-2.
Hypercapnia is caused by inadequate alveolar ventilation. Potential contributing factors include (1) increased CO2 production, (2) decreased ventilatory drive, (3) malfunction of the respiratory pump or increased airway resistance, and (4) inefficiency of gas exchange (increased dead space or ventilation/perfusion mismatch).
Although diffusion abnormalities rarely cause hypoxemia at rest, assessment of DLCO can be used to determine the functional integrity of the alveolar-capillary membrane. Diseases that solely affect the airways typically do not reduce the DLCO. DLCO is reduced in interstitial lung disease, emphysema, and pulmonary vascular disease. DLCO can be elevated in alveolar hemorrhage, asthma, and congestive heart failure.
Outline