WorkupFor active IK or old, previously untreated IK:
- History: Venereal disease in the mother during pregnancy or in the patient? Hearing loss or tinnitus? Prior HSV or shingles infections?
- External examination: Look for saddle-nose deformity, Hutchinson teeth, frontal bossing, or other signs of congenital syphilis. Look for hypopigmented or anesthetic skin lesions and thickened skin folds, loss of the temporal eyebrow, and loss of eyelashes, as in leprosy.
- Slit lamp examination: Examine corneal nerves for segmental thickening, like beads on a string (leprosy). Examine the iris for nodules (leprosy) and hyperemia with fleshy, pink nodules (syphilis). Check IOP.
- Dilated fundus examination: Look for classic salt-and-pepper chorioretinitis or optic atrophy of syphilis.
- Laboratory evaluation: Fluorescent treponemal antibody absorption (FTA-ABS) or treponemal-specific assay (e.g., microhemagglutination-Treponema pallidum [MHA-TP]) for prior exposure; Venereal Disease Research Laboratory test (VDRL) or rapid plasma reagin (RPR) for disease activity. See 12.12, SYPHILIS.
- Purified protein derivative (PPD) or interferon-gamma release assay (IGRA) (e.g., QuantiFERON-TB Gold),
- Lyme serology if in endemic region.
- Chest radiograph or chest CT if negative FTA-ABS (or MHA-TP) or positive PPD or IGRA.
- Consider erythrocyte sedimentation rate, rheumatoid factor, complete blood count, and EBV antibody.
- Acute disease: Every 3 to 7 days initially, and then every 2 to 4 weeks. The frequency of steroid administration is slowly reduced as the inflammation subsides over the course of months (may take years). IOP is monitored closely and reduced with medications based on the degree of IOP elevation and overall health of the optic nerve (see 9.7, INFLAMMATORY OPEN ANGLE GLAUCOMA).
- Old inactive disease: Yearly follow up, unless treatment is required for underlying etiology.
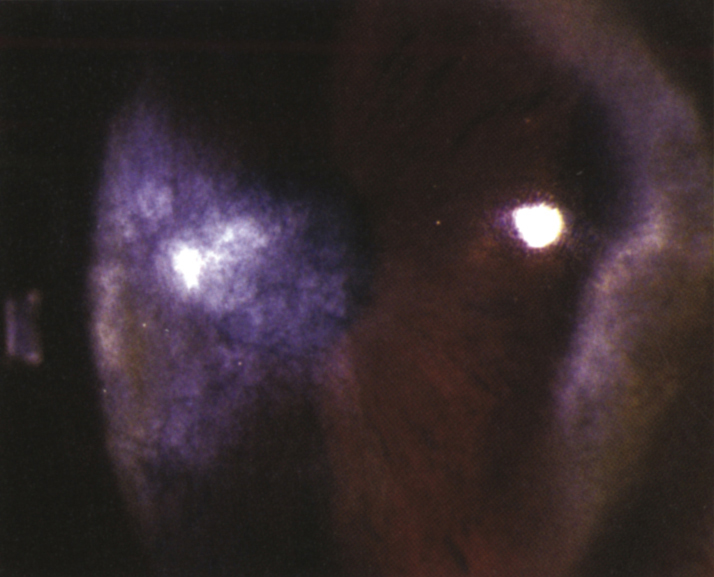
IK is broadly defined as any non-ulcerating inflammation of the corneal stroma without epithelial or endothelial involvement, but often with neovascularization. IK is the common end-point of many corneal diseases.