Red eye, pain, foreign body sensation, photophobia, tearing, decreased vision, skin (e.g., eyelid) vesicular rash, history of previous episodes; usually unilateral.
Primary HSV infection is usually not apparent clinically. However, neonatal primary herpes infection is a rare, potentially devastating disease associated with localized skin, eye, or oral infection and severe central nervous system and multiorgan system infection (see 8.9, OPHTHALMIA NEONATORUM [NEWBORN CONJUNCTIVITIS]). Compared to adults, children tend to exhibit more severe disease that may be bilateral, recurrent, and associated with extensive eyelid involvement, multiple corneal/conjunctival dendrites, and a greater degree of secondary corneal scarring and astigmatism. Possible triggers for recurrence include ocular surgery, certain topical medications, fever, stress, menstruation, and upper respiratory tract infection. Infection may be characterized by any or all of the following:
Eyelid/Skin Involvement
Clear vesicles on an erythematous base that progress to crusting, heal without scarring, cross dermatomes, but are typically unilateral (only 10% of primary HSV dermatitis is bilateral).
Conjunctivitis
Conjunctival injection with acute unilateral follicular conjunctivitis, with or without conjunctival dendrites or geographic ulceration.
Epithelial Keratitis
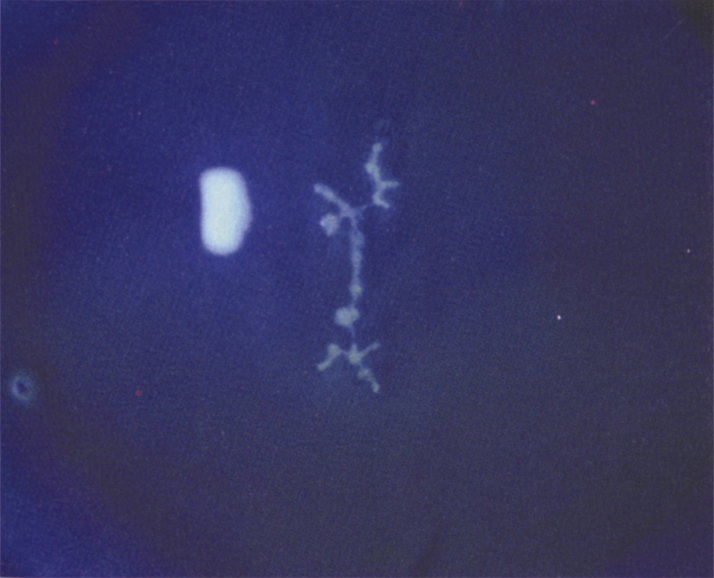
(See Figure 4.15.1.)
May be seen as macropunctate keratitis, dendritic keratitis (a thin, linear, branching epithelial ulceration with club-shaped terminal bulbs at the end of each branch), or a geographic ulcer (a large, amoeba-shaped corneal ulcer with a dendritic edge). The edges of herpetic lesions are heaped up with swollen epithelial cells that stain well with rose bengal or lissamine green; the central ulceration stains well with fluorescein. Corneal sensitivity may be decreased. Subepithelial scars and haze (ghost dendrites) may develop as epithelial dendrites resolve. Epithelial keratitis is considered to be live, replicating viral disease, and treatment is directed accordingly.
Differential Diagnosis of Corneal DendritesA “true” dendrite (branching epithelial ulceration with terminal end-bulbs) is pathognomonic for HSV however there are many similar appearing lesions that should be distinguished:
- VZV: Pseudodendrites in VZV are slightly elevated and are without central ulceration. They do not have true terminal bulbs and do not typically stain well with fluorescein. See 4.16, HERPES ZOSTER OPHTHALMICUS/VARICELLA ZOSTER VIRUS.
- Recurrent corneal erosion or any recent corneal abrasion: A healing epithelial defect often has a dendritiform appearance. Recurrent erosions in patients with lattice dystrophy can have a geographic shape. See 4.2, RECURRENT CORNEAL EROSION.
- Acanthamoeba keratitis pseudodendrites: History of soft contact lens wear, pain often out of proportion to inflammation, chronic course. These are raised epithelial lesions, not epithelial ulcerations. See 4.13, ACANTHAMOEBA KERATITIS.
- Others: Cornea verticillata from medications or Fabry disease, and rarely tyrosinemia.
Stromal Keratitis
- Stromal keratitis without ulceration (alternate terms: nonnecrotizing keratitis, immune stromal keratitis, interstitial keratitis): Unifocal or multifocal stromal haze or whitening, often with stromal edema, in the absence of epithelial ulceration. Accompanying stromal vascularization indicates chronicity or prior episodes. The differential of stromal keratitis without ulceration includes any cause of IK (see below). HSV stromal keratitis is considered an immune reaction rather than active infectious process and therefore treatment is directed accordingly.
- Stromal keratitis with ulceration (necrotizing keratitis): Suppurative stromal inflammation, thinning, with an adjacent or overlying epithelial defect. Appearance may be indistinguishable from infectious keratitis (fungal, bacterial, parasitic) and therefore infection should be ruled out. Stromal keratitis may lead to thinning or scarring and therefore must be treated diligently.
- Endothelial keratitis (disciform keratitis): Corneal stromal and epithelial edema in a round or discrete pattern, associated with an area of keratic precipitates often out of proportion to the amount of anterior chamber inflammation.
Neurotrophic Ulcer
- A chronic presentation in a relatively neurotrophic cornea due to fifth cranial nerve sensory damage following prior keratitis. A sterile ulcer with smooth epithelial margins over an area of interpalpebral stromal disease that persists or worsens despite antiviral therapy. May be associated with stromal melting and perforation. Without a known history or HSV keratitis, other causes of neurotrophic keratitis should be considered, including: VZV, diabetes, cranial surgery, or radiation.
Uveitis
- An anterior chamber inflammatory reaction may develop during corneal stromal disease or independently from keratitis. Elevated IOP secondary to trabeculitis is often suggestive of herpetic uveitis. Patchy iris transillumination defects are also characteristic.