Dermatomal pain, paresthesias, and skin rash or discomfort. May be preceded by headache, fever, or malaise, and accompanied or followed by blurred vision, eye pain, and red eye.
See Table 4.16.1.
 NOTE: NOTE: |
Immunocompromised patients should not receive systemic steroids. |
Skin Involvement
- In adults with a moderate-to-severe skin rash for <4 days in which active skin lesions are present and consider if the patient presents later in the first week with active lesions:
- Oral antiviral agent (e.g., acyclovir 800 mg p.o. five times per day, valacyclovir 1,000 mg p.o. t.i.d., or famciclovir 500 mg p.o. t.i.d.) for 7 to 10 days. If the condition is severe, as manifested by orbital, optic nerve, or cranial nerve involvement, or the patient is systemically ill, hospitalize and prescribe acyclovir 5 to 10 mg/kg i.v. q8h for 5 to 10 days.
- Ophthalmic antibiotic ointment (e.g., bacitracin or erythromycin) to skin lesions b.i.d.
- Warm compresses to periocular skin t.i.d.
- Adults with a skin rash of more than 1-week duration or without active skin lesions:
- Ophthalmic antibiotic ointment (e.g., bacitracin or erythromycin) to skin lesions b.i.d.
- Warm compresses to periocular skin t.i.d.
- Children: Discuss with a pediatrician and consider weight-based acyclovir dosing (20 mg/kg q8h) for children <12 years of age or under 40 kg, otherwise use adult dosage above. For systemic spread, hospitalize and prescribe intravenous acyclovir in conjunction with pediatric and infectious disease comanagement.
Ocular Involvement
 NOTE: NOTE: |
It is common clinical practice at Wills Eye for all patients with VZV ocular findings to receive 7 to 10 days of systemic oral antivirals (e.g., acyclovir 800 mg p.o. five times per day, valacyclovir 1,000 mg p.o. t.i.d., or famciclovir 500 mg p.o. t.i.d.) usually in conjunction with the following therapies. |
- Conjunctival involvement: Cool compresses and ophthalmic ointment (e.g., bacitracin or erythromycin) to the eye b.i.d.
- SPK: Lubrication with preservative-free artificial tears q1–2h and ointment q.h.s.
- Corneal or conjunctival mucous plaque pseudodendrites: Lubrication with preservative-free artificial tears q1–2h and ointment q.h.s. Consider antibiotic ointment to prevent bacterial superinfection. Topical antivirals (e.g., ganiciclovir gel four to five times daily) may be helpful for recalcitrant corneal mucous plaque pseudodendrites.
- Immune stromal keratitis: Topical steroid (e.g., prednisolone acetate 1%) started at a frequency of four to eight times per day and adjusted according to clinical response. Topical steroids are tapered over months to years using weaker steroids with a goal of less than daily dosing (e.g., q.o.d., twice weekly, once weekly, etc.).
- Uveitis (with or without immune stromal keratitis): Topical steroid (e.g., prednisolone acetate 1%) four to eight times per day and cycloplegic drop (e.g., cyclopentolate 1% t.i.d.). See 12.1, ANTERIOR UVEITIS (IRITIS/IRIDOCYCLITIS). Treat increased IOP with aggressive aqueous suppression; avoid prostaglandin analogues.
- Neurotrophic keratitis: Treat mild epithelial defects with ophthalmic antibiotic ointment (e.g., erythromycin) four to eight times per day. If a corneal infiltrate occurs, obtain appropriate smears and cultures to rule out infection (see 4.11, BACTERIAL KERATITIS). If the infiltrate is sterile, and there is no response to ointment, consider punctal plugs, bandage soft contact lens, tarsorrhaphy, amniotic membrane tissue, autologous serum tears, recombinant nerve growth factor, or conjunctival flap along with prophylactic topical antibiotics (see 4.6, NEUROTROPHIC KERATOPATHY).
- Scleritis: See 5.7, SCLERITIS.
- Retinitis, choroiditis, optic neuritis, or cranial nerve palsy: Acyclovir 10 mg/kg i.v. q8h for 1 week and prednisone 60 mg p.o. for 3 days, then taper over 1 week. Management of ARN or PORN may require intraocular antivirals (see 12.8, ACUTE RETINAL NECROSIS). Infectious disease and neurologic consultation to rule out central nervous system involvement should be considered. Patients with severe disease can develop a large vessel cranial arteritis resulting in a massive cerebrovascular accident.
- Increased IOP: May be steroid response or secondary to inflammation. If uveitis is present, increase the frequency of the steroid administration for a few days and use topical aqueous suppressants (e.g., timolol 0.5% daily or b.i.d., brimonidine 0.2% t.i.d., or dorzolamide 2% t.i.d.; see 9.7, INFLAMMATORY OPEN ANGLE GLAUCOMA, and 9.9, STEROID-RESPONSE GLAUCOMA). Oral carbonic anhydrase inhibitors may be necessary if the IOP is >30 mm Hg. If IOP remains increased and the inflammation is controlled, substitute fluorometholone 0.1% or loteprednol 0.5% drops for prednisolone acetate and attempt to taper the dose.
 NOTE: NOTE: |
Pain may be severe during the first 2 weeks, and narcotic analgesics may be required. An antidepressant (e.g., amitriptyline 25 mg p.o. t.i.d.) may be beneficial for both postherpetic neuralgia and depression that can develop in VZV. Capsaicin 0.025% or doxepin ointment may be applied to the skin t.i.d. to q.i.d. after the rash heals (not around the eyes) for postherpetic neuralgia. Oral gabapentin or pregabalin can be helpful for acute pain and for postherpetic neuralgia. Management of postherpetic neuralgia should involve the patient’s primary medical doctor or a pain management specialist. |
4-16.1 Antiviral Therapy Guidelines for Varicella Zoster Virus
| Drug | Dosing Information | Toxicities | Contraindications |
|---|
| Acyclovir | If immunocompetent, 800 mg p.o. five times per day; if immunocompromised, start 10/mg/kg i.v. q8h (q12h if creatinine >2.0) for 7 to 10 d, followed by 800 mg p.o. five times per day to prevent reactivation. | Intravenous: reversible renal and neurologic toxicity | Use with caution in patients with a history of renal impairment. | | Famciclovir | 500 mg p.o. q8h. Adjust dosage for creatinine clearance <60 mL/min. | Headache, nausea, diarrhea, dizziness, fatigue | Use with caution in patients with a history of renal impairment. | | Valacyclovir | 1 g p.o. q8h. Adjust dosage for creatinine clearance <60 mL/min. | Headache, nausea, vomiting, diarrhea | TTP/HUS has been reported in patients with advanced HIV/AIDS. |
|
If ocular involvement is present, examine the patient every 1 to 7 days, depending on the severity. Patients without ocular involvement can be followed every 1 to 4 weeks. After the acute episode resolves, check the patient every 3 to 6 months (3 if on steroids) because relapses may occur months to years later, particularly as steroids are tapered. Systemic steroid use is controversial.
 NOTE: NOTE: |
VZV is contagious for children and adults who have not had chickenpox or the chickenpox vaccine and is spread by inhalation. Varicella-naïve pregnant women must be especially careful to avoid contact with a VZV-infected patient. A vaccine for shingles is recommended for people aged 50 years or older. |
Varicella Zoster Virus (Chickenpox)
Symptoms
Facial rash, red eye, foreign body sensation.
Signs
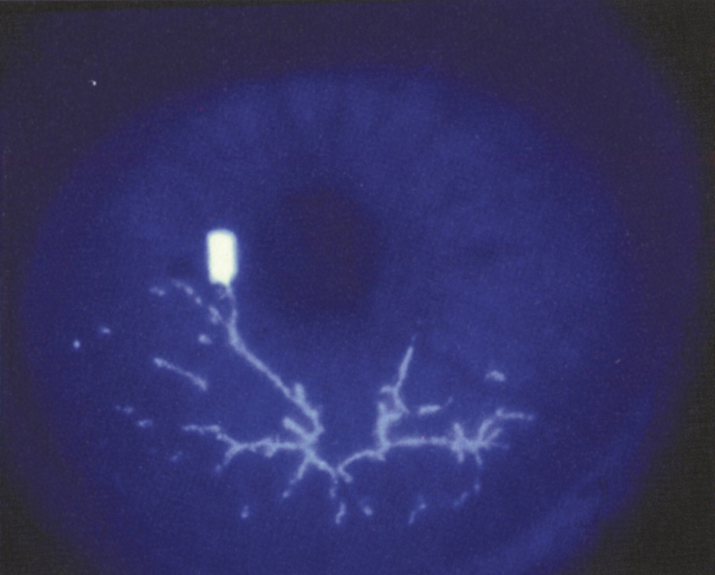
Early: Acute conjunctivitis with vesicles or papules at the limbus, on the eyelid, or on the conjunctiva. Pseudodendritic corneal epithelial lesions, stromal keratitis, anterior uveitis, optic neuritis, retinitis, and ophthalmoplegia occur rarely.
Late: Immune stromal or neurotrophic keratitis.
Treatment
- Conjunctival involvement and/or corneal epithelial lesions: Cool compresses and ophthalmic antibiotic ointment (e.g., erythromycin t.i.d.) to the eye and periorbital lesions.
- Stromal keratitis with uveitis: Topical steroid (e.g., prednisolone acetate 1% q.i.d.), cycloplegic drop (e.g., cyclopentolate 1% t.i.d.)
- Neurotrophic keratitis: Uncommon; see 4.6, NEUROTROPHIC KERATOPATHY.
- Canalicular obstruction: Uncommon. Managed by intubation of puncta.
 NOTE: NOTE: |
- Aspirin is contraindicated in children because of the risk of Reye syndrome.
- Immunocompromised children with chickenpox may require i.v. acyclovir.
|
Follow Up
- Follow up in 1 to 7 days, depending on the severity of ocular disease. Taper the topical steroids slowly.
- Watch for stromal or neurotrophic keratitis approximately 4 to 6 weeks after the chicken pox infection resolves.