Variable decreased vision (typically around 20/200 level for a full-thickness hole, better for a partial-thickness hole), metamorphopsia, or central scotoma. Three times more likely in women; usually occurs in sixth to eighth decade. 10% bilateral.
(See Figures 11.25.1 and 11.25.2.)
Critical
A full-thickness macular hole appears as a round, red spot in the center of the macula, usually from one-third to two-thirds of a disc diameter in size; may be surrounded by a gray halo/cuff of SRF. Vitreomacular traction (VMT) demonstrates loss of the normal foveolar depression and often a yellow spot or ring in the center of the macula.
Other
Small, yellow precipitates deep to the retina in the hole or surrounding retina; retinal cysts at the margin of the hole or a small operculum above the hole, anterior to the retina (Gass stage 3 or 4); or both.
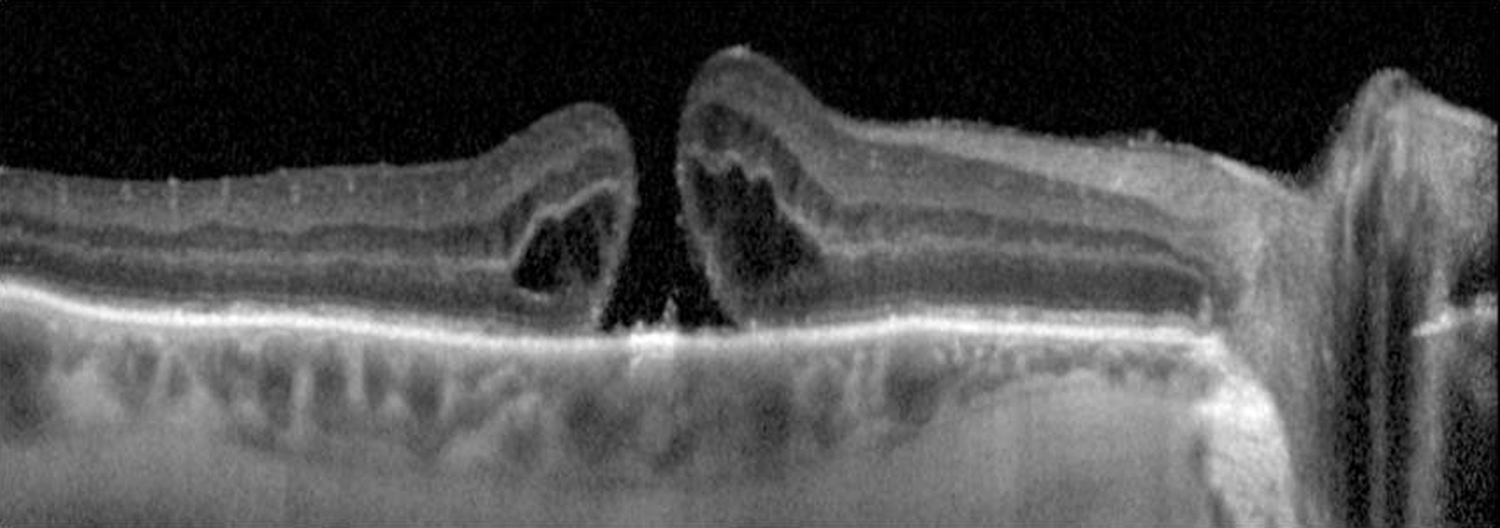
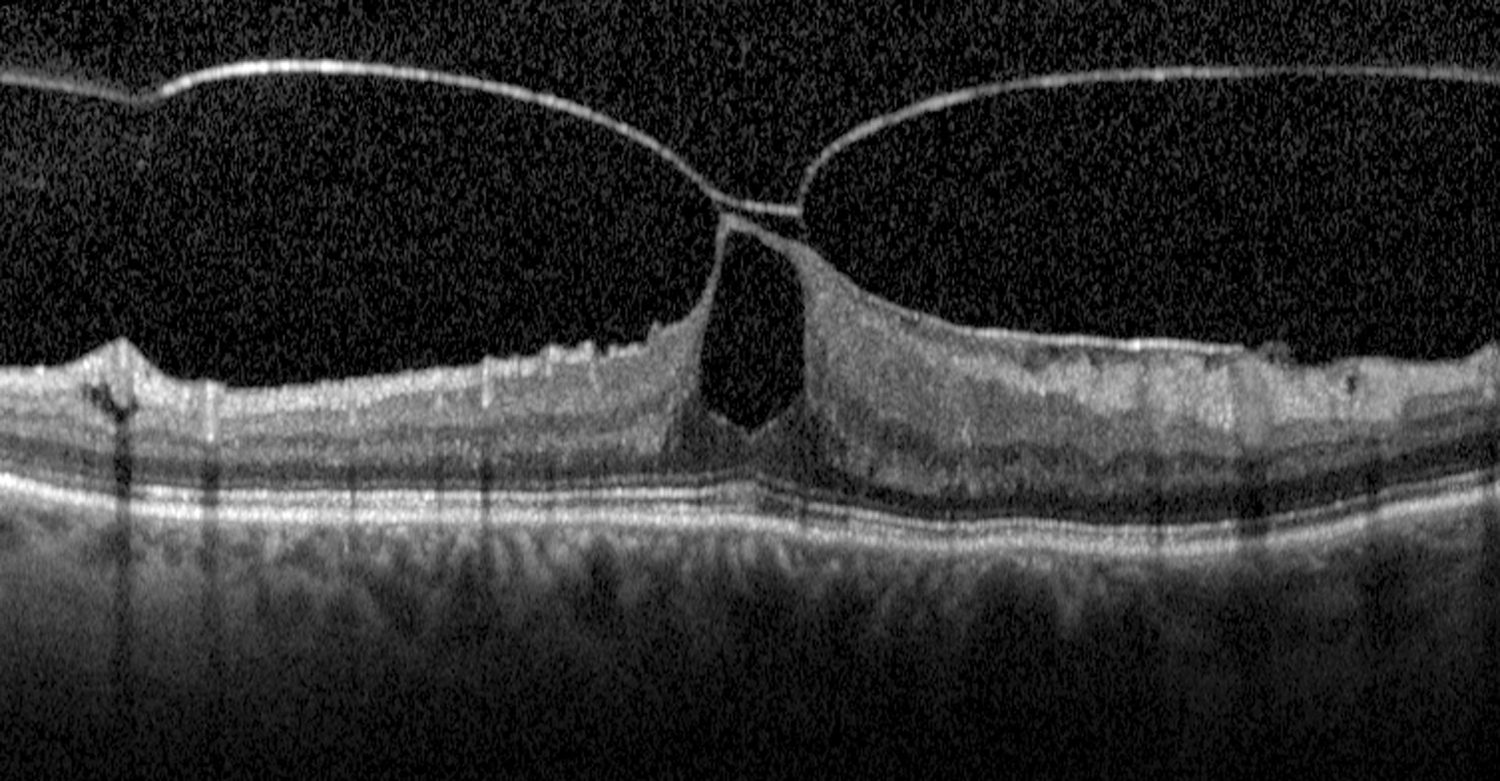
11-25.2 Optical coherence tomography of macular hole.
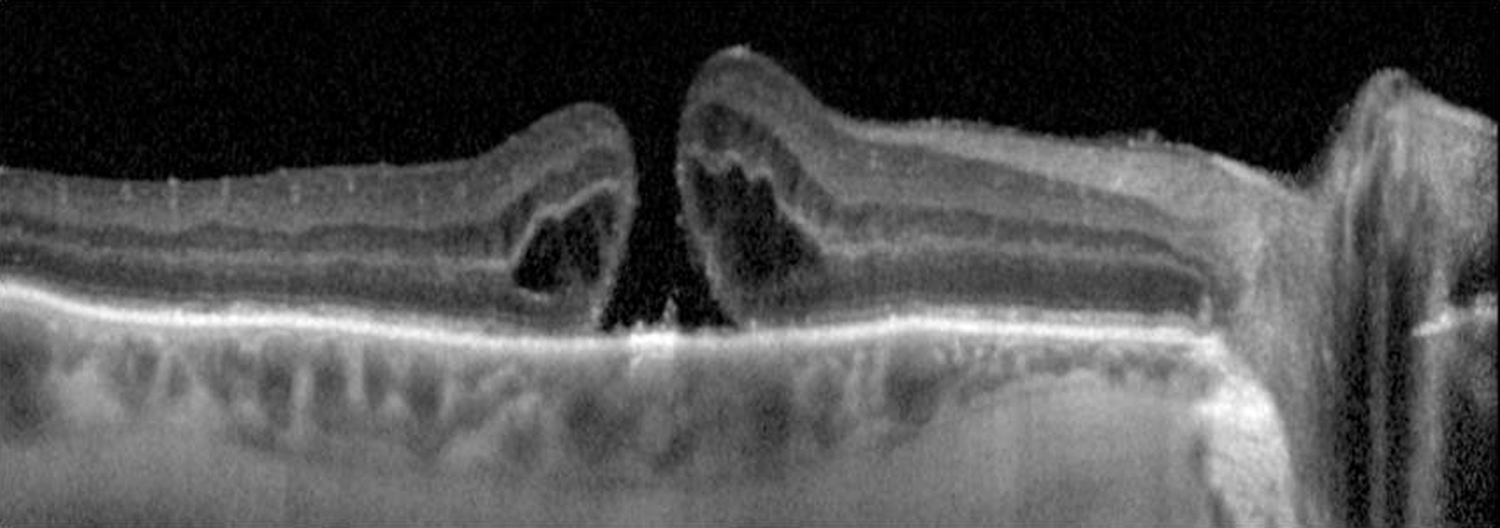
11-25.1 Macular hole.

Gass Staging of Macular Hole
- Stage 1: An impending hole, yellow spot, or ring in fovea.
- Stage 2: Small full-thickness hole.
- Stage 3: Full-thickness hole with cuff of SRF, no PVD.
- Stage 4: Full-thickness hole with cuff of SRF, with complete PVD.
 NOTE: NOTE: |
A new classification system using OCT has been developed. It is based on size of the full-thickness hole, presence of VMT, and underlying etiology (e.g., primary VMT versus secondary trauma). |
May be difficult to distinguish a macular hole from a pseudohole (no loss of foveal tissue) or a lamellar macular hole (partial-thickness).
- Macular pucker with a pseudohole: An ERM (surface-wrinkling) on the surface of the retina may simulate a macular hole. See 11.26, EPIRETINAL MEMBRANE (MACULAR PUCKER, SURFACE-WRINKLING RETINOPATHY, CELLOPHANE MACULOPATHY). Look for a sheen from ILM changes or ERM.
- Lamellar hole: Not as red as a full-thickness hole, and a surrounding gray halo is usually not present.
- Intraretinal cysts (e.g., chronic CME with prominent central cyst).
- Solar retinopathy: Small, round, red or yellow lesion at the center of the fovea, with surrounding fine gray pigment in a sun gazer or eclipse watcher. See 11.35, SOLAR RETINOPATHY.
May be caused by vitreous or ERM traction on the macula, trauma, or CME. In early stages of vitreomacular adhesion (VMA)/VMT, the vitreous cortex is attached to the fovea but detached from the perifoveal region, exerting anteroposterior traction on the fovea. Increased tractional forces can allow for eventual progression to full-thickness macular hole.
Duker JS, Kaiser PK, Binder S, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120(12):2611-2619.