Critical
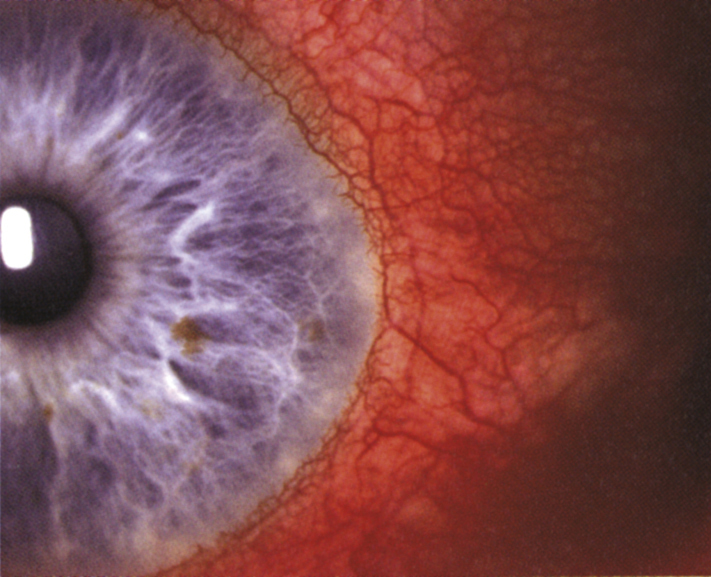
Sectoral (and, less commonly, diffuse) redness of one or both eyes, mostly due to engorgement of the episcleral vessels. These vessels are large, run in a radial direction beneath the conjunctiva, and can be moved slightly with a cotton-tip applicator (see Figure 5.6.1).
Other
Mild-to-moderate tenderness over the area of episcleral injection or a nodule that can be moved slightly over the underlying sclera may be seen. Fluorescein staining can sometimes be seen over the nodule. Associated anterior uveitis and corneal involvement are rare. Vision is normal.