Visual acuity usually normal. Often asymptomatic.
Thought to be an acute obstruction of a precapillary retinal arteriole causing blockage of axoplasmic flow and subsequent buildup of axoplasmic debris in the NFL.
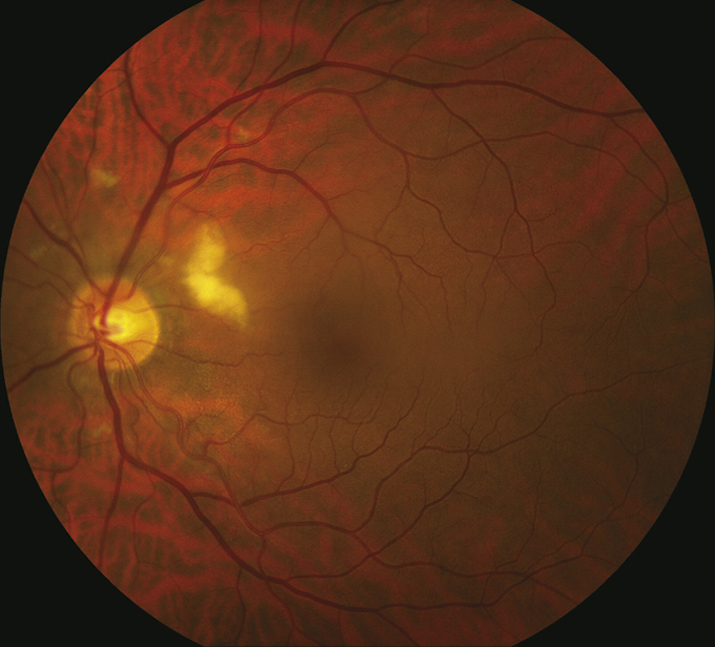
- Diabetes mellitus: Most common cause. Often associated with microaneurysms, dot-blot hemorrhages, and hard exudates. See 11.12, DIABETIC RETINOPATHY.
- Chronic or acute HTN: May see retinal arteriolar narrowing and flame hemorrhages in chronic HTN. Acute HTN may have hard exudates, optic nerve swelling, exudative RD. See 11.10, HYPERTENSIVE RETINOPATHY.
- Retinal vein occlusion: Unilateral, multiple hemorrhages, venous dilation, and tortuosity. Multiple CWSs, usually ≥6, seen in ischemic varieties. See 11.8, CENTRAL RETINAL VEIN OCCLUSION and 11.9, BRANCH RETINAL VEIN OCCLUSION.
- Retinal emboli: Often from carotid arteries or heart with resulting ischemia and subsequent CWS distal to arterial occlusion. Patients require carotid Doppler examination and echocardiography. See 10.22, TRANSIENT VISUAL LOSS/AMAUROSIS FUGAX.
- Collagen vascular disease: Systemic lupus erythematosus (most common), granulomatosis with polyangiitis (formerly Wegener granulomatosis), polyarteritis nodosa, scleroderma, etc.
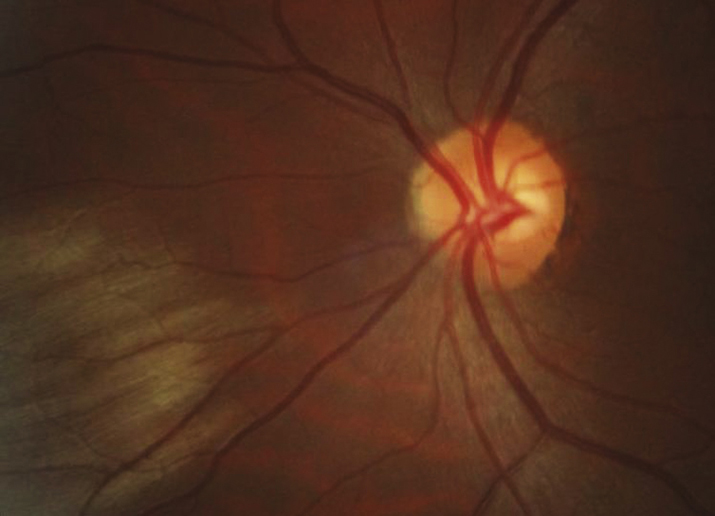
- Giant cell arteritis (GCA): Age ≥55 years. Symptoms include vision loss, scalp tenderness, jaw claudication, proximal muscle aches, etc. See 10.17, ARTERITIC ISCHEMIC OPTIC NEUROPATHY (GIANT CELL ARTERITIS).
- HIV retinopathy: Single or multiple CWSs in the posterior pole. See 12.10, NONINFECTIOUS RETINAL MICROVASCULOPATHY/HIV RETINOPATHY.
- Other infections: Toxoplasmosis, orbital zygomycosis, Lyme disease, leptospirosis, Rocky Mountain spotted fever, onchocerciasis, subacute bacterial endocarditis, others.
- Hypercoagulable state: Polycythemia, multiple myeloma, cryoglobulinemia, Waldenström macroglobulinemia, antiphospholipid syndrome, factor V Leiden, activated protein C resistance, hyperhomocysteinemia, protein C and S deficiency, antithrombin III mutation, prothrombin mutation, etc.
- Radiation retinopathy: Follows radiation therapy to the eye or periocular structures when the eye is irradiated inadvertently. May occur any time after radiation, but occurs most commonly within a few years. Maintain a high suspicion even in patients in whom the eye was reportedly shielded. Usually, 3,000 cGy is necessary, but it has been noted to occur with 1,500 cGy. Resembles diabetic retinopathy.
- Interferon therapy.
- Purtscher and pseudo-Purtscher retinopathy: Multiple CWSs and/or superficial hemorrhages in a peripapillary configuration. Typically bilateral but can be unilateral and asymmetric. See 3.20, PURTSCHER RETINOPATHY.
- Cancer: Metastatic carcinoma, leukemia, lymphoma, others.
- Others: Migraine, hypotension, intravenous drug use, papilledema, papillitis, severe anemia, sickle cell, acute blood loss, etc.
Identify and treat underlying etiology.
Depends on underlying etiology. If concern for infectious process, serial dilated examinations are recommended. CWSs typically fade in 5 to 7 weeks but can remain longer if associated with diabetic retinopathy.