Critical
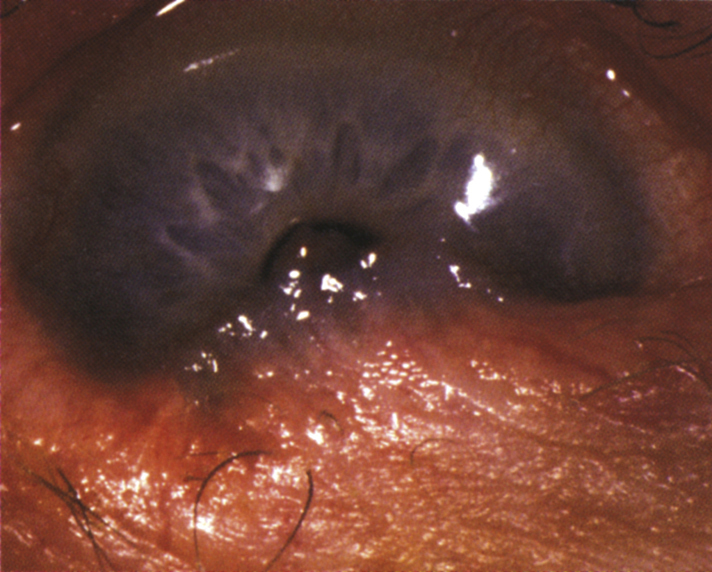
Inferior symblepharon (linear folds of conjunctiva connecting the palpebral conjunctiva of the lower eyelid to the inferior bulbar conjunctiva), foreshortening and tightness of the lower fornix, and scarring of palpebral conjunctiva on eyelid eversion (see Figure 5.10.1).
Other
Secondary bacterial conjunctivitis, SPK, and corneal ulcer. Potential later findings include poor tear film, resulting in severe dry eye syndrome; entropion; trichiasis or distichiasis (if present, carefully examine fornices for symblepharon); corneal opacification with pannus, neovascularization, and keratinization; obliteration of the fornices, with eventual limitation of ocular motility; and ankyloblepharon.
Systemic
Mucous membrane (e.g., oropharynx, esophagus, anus, vagina, and urethra) vesicles; scarring or strictures; ruptured or formed bullae; denuded epithelium. Desquamative gingivitis is common. Cutaneous vesicles and bullae may occur, sometimes with erythematous plaques or scars near affected mucous membranes.
Based on clinical findings, the disease can be divided into four stages:
- Stage I—Chronic conjunctivitis with mild corneal involvement.
- Stage II—Cicatrization with conjunctival shrinkage and foreshortening of fornices.
- Stage III—Above with the additional presence of symblepharon. Subepithelial scarring leads to distortion of lashes.
- Stage IV—End stage, with ankyloblepharon and severe corneal involvement (persistent epithelial defects, stromal ulcers, scarring, neovascularization, and diffuse keratinization).