Partial-Thickness Laceration
Workup
- Careful slit lamp examination should be performed to exclude ocular penetration. Carefully evaluate the conjunctiva, sclera, and cornea, checking for extension beyond the limbus in cases involving the corneal periphery. Evaluate AC depth and compare with the fellow eye. A shallow AC indicates an actively leaking wound or a self-sealed leak (see FULL-THICKNESS CORNEAL LACERATION below). Check for iris TIDs and evaluate the lens for a cataract or a foreign body tract (must have a high level of suspicion with projectile objects). The presence of TIDs and lens abnormalities indicates a ruptured globe.
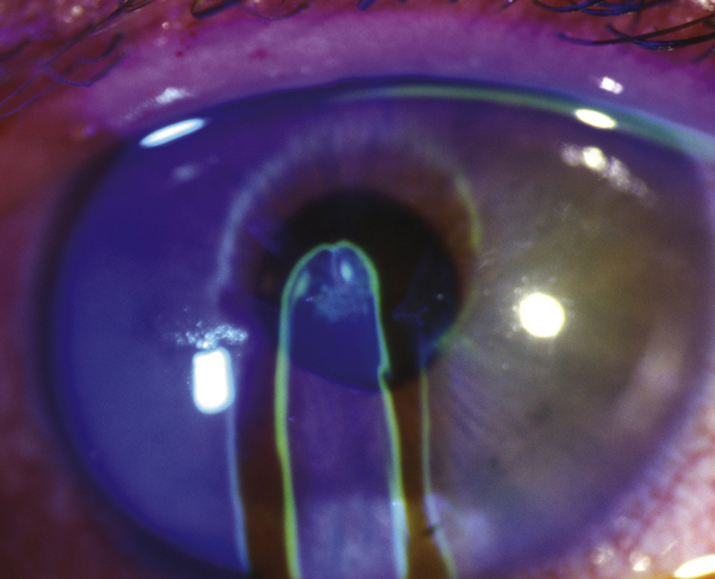
- Seidel test (see APPENDIX 5, SEIDEL TEST TO DETECT A WOUND LEAK). If the Seidel test is positive, a full-thickness laceration is present (see FULL-THICKNESS CORNEAL LACERATION below). A negative Seidel test indicates either a partial-thickness laceration or a self-sealed full-thickness laceration.
- Avoid IOP measurement if the Seidel test is positive. Measure IOP with caution if the Seidel test is negative to avoid opening a previously self-sealed full-thickness laceration.
Treatment
- A cycloplegic (e.g., cyclopentolate 1% to 2%) and frequent application of an antibiotic (e.g., polymyxin B/bacitracin ointment or fluoroquinolone drops) depending on the nature of the wound.
- When a moderate to deep corneal laceration is accompanied by wound gape, it is often best to suture the wound closed in the operating room to provide structural stability and to avoid excessive scarring with corneal irregularity, especially when in the visual axis.
- If corneal foreign bodies are present and superficial, treat per Sections 3.3, CORNEAL AND CONJUNCTIVAL FOREIGN BODIES. If foreign bodies are in the deeper cornea, there are no signs of infection or inflammation, and are well tolerated (see 3.15, INTRAOCULAR FOREIGN BODY, for inert foreign bodies), they may be left and watched closely. If the patient is symptomatic or if signs of infection/inflammation occur, deeper corneal foreign bodies should be removed in the operating room.
- Tetanus toxoid for dirty wounds (see APPENDIX 2, TETANUS PROPHYLAXIS).
Follow Up
Reevaluate daily until the epithelium heals.
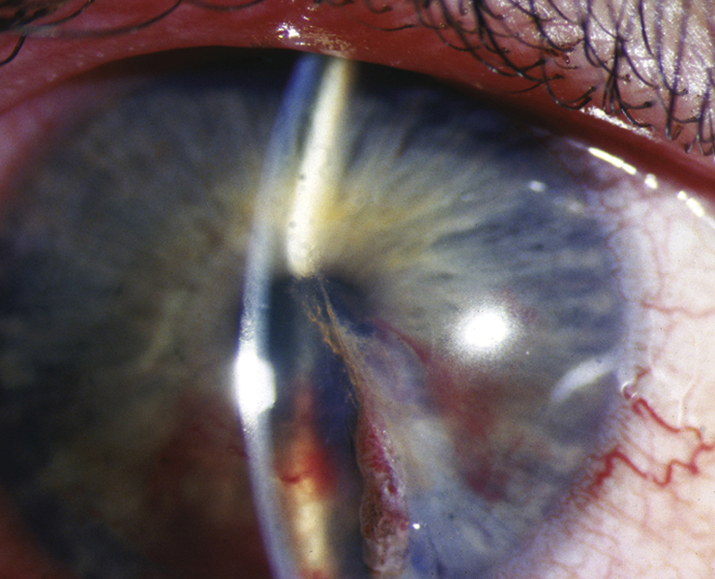
Full-Thickness Corneal Laceration
(See Figure 3.13.2.)
See 3.14, RUPTURED GLOBE AND PENETRATING OCULAR INJURY. Note that small, self-sealing, or slow-leaking lacerations with formed ACs may be treated with aqueous suppressants, bandage soft contact lenses, fluoroquinolone drops q.i.d., and precautions as listed in Sections 3.14, RUPTURED GLOBE AND PENETRATING OCULAR INJURY. Avoid topical steroids. If an IOFB is present, see 3.15, INTRAOCULAR FOREIGN BODY.