Symptoms
Foreign body sensation, tearing, pain, and redness.
Signs
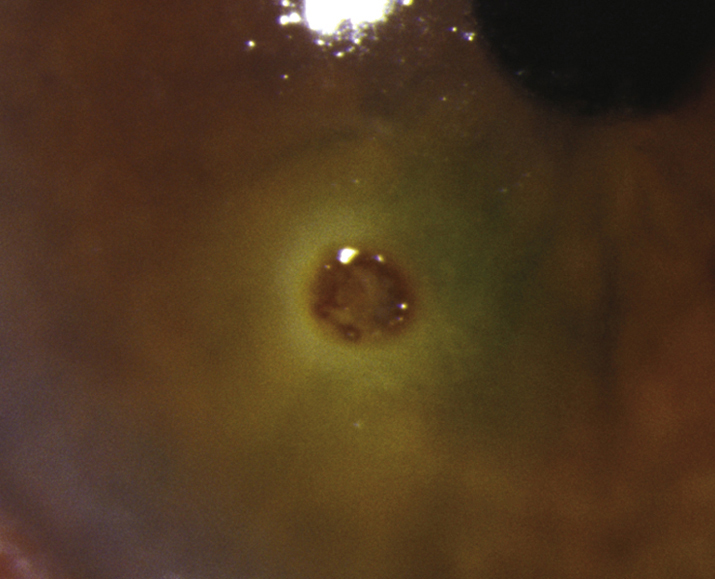
(See Figure 3.3.1.)
Critical
Conjunctival or corneal foreign body with or without a rust ring.
Other
Conjunctival injection, eyelid edema, mild AC reaction, and SPK. A small infiltrate may surround a corneal foreign body; it is usually reactive and sterile. Vertically oriented linear corneal abrasions or SPK may indicate a foreign body under the upper eyelid.
Workup
- History: Determine the mechanism of injury (e.g., metal striking metal, power tools or weed-whackers, direct pathway with no safety glasses, distance of the patient from the instrument of injury, etc.). Attempt to determine the size, shape, velocity, force, and composition of the object. Always keep in mind the possibility of an intraocular foreign body (IOFB).
- Document visual acuity before any procedure is performed. One or two drops of topical anesthetic may be necessary to facilitate the examination.
- Slit lamp examination: Locate and assess the depth of the foreign body. Examine closely for possible entry sites (rule out self-sealing lacerations), pupil irregularities, iris tears and transillumination defects (TIDs), lens capsular perforations, lens opacities, hyphema, AC shallowing (or deepening in scleral perforations), and asymmetrically low IOP in the involved eye.
If there is no evidence of perforation, evert the eyelids and inspect the fornices for additional foreign bodies. Double everting the upper eyelid with a Desmarres eyelid retractor may be necessary. Carefully inspect conjunctival lacerations to rule out an underlying scleral laceration or perforation. Measure and diagram the dimensions of any corneal or scleral infiltrate and the degree of any AC reaction for monitoring therapy response and progression of possible infection.
- Dilate the eye and examine the posterior segment for possible IOFB (see 3.15, INTRAOCULAR FOREIGN BODY).
- Consider B-scan ultrasonography, computed tomography (CT) scan of the orbit (axial, coronal, and parasagittal views, 1-mm sections), or ultrasound biomicroscopy (UBM) to exclude an intraocular or intraorbital foreign body. While we prefer a CT scan, a plain film x-ray can also be used to rule out radiodense foreign bodies. Avoid magnetic resonance imaging (MRI) if there is a history of possible metallic foreign body.
There may be multiple foreign bodies with injuries due to power equipment or explosive debris. |
An infiltrate accompanied by a significant AC reaction, purulent discharge, or extreme conjunctival injection and pain should be cultured to rule out infection, treated aggressively with antibiotics, and followed closely (see 4.11, BACTERIAL KERATITIS). |
Treatment
Corneal Foreign Body (Superficial or Partial Thickness)
- Apply topical anesthetic (e.g., proparacaine). Remove the corneal foreign body with a foreign body spud or fine forceps such as jeweler’s forceps at a slit lamp. Multiple superficial foreign bodies may be more easily removed by irrigation.
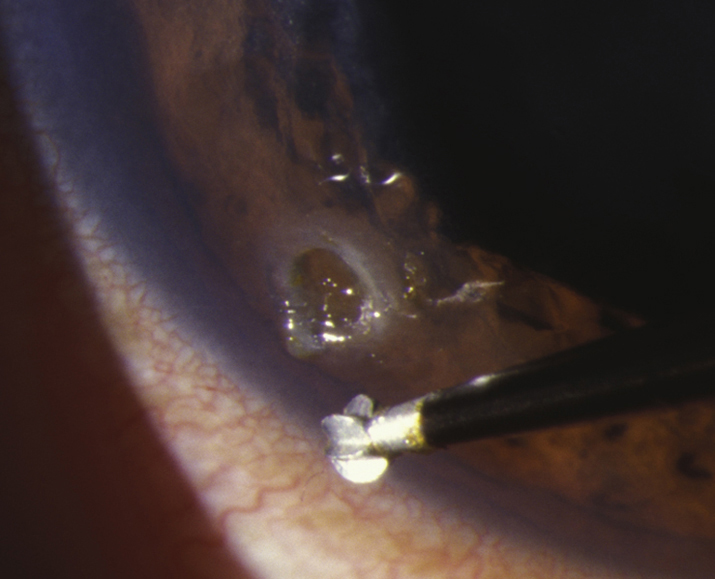
- Remove the rust ring as completely as possible on the first visit. This may require an ophthalmic burr (see Figure 3.3.2). It is sometimes safer to leave a deep, central rust ring to allow time for the rust to migrate to the corneal surface, at which point it can be removed more easily.
- Measure and diagram the size of the resultant corneal epithelial defect.
- Treat as indicated for corneal abrasion (see 3.2, CORNEAL ABRASION).
- Alert the patient to return as soon as possible if there is any worsening of symptoms.
- Counsel patient about protective eye wear.
If there is concern for full-thickness corneal foreign body, exploration and removal should be performed in the operating room. |
Erythromycin ointment should not be used for residual epithelial defects from corneal foreign bodies as it does not provide strong enough antibiotic coverage. |
Conjunctival Foreign Body
- Remove foreign body under topical anesthesia.
- Multiple or loose superficial foreign bodies can often be removed with saline irrigation.
- A foreign body can be removed with a cotton-tipped applicator soaked in topical anesthetic or with fine forceps. For deeply embedded foreign bodies, consider pretreatment with a cotton-tipped applicator soaked in phenylephrine 2.5% to reduce conjunctival bleeding.
- Small, relatively inaccessible, buried subconjunctival foreign bodies may sometimes be left in the eye without harm unless they are infectious or proinflammatory. Occasionally, they will surface with time, at which point they may be removed more easily. Conjunctival excision is sometimes indicated.
- Check the pH if an associated chemical injury is suspected (e.g., alkali from fireworks). See 3.1, CHEMICAL BURN.
- Sweep the conjunctival fornices with a cotton-tipped applicator soaked with a topical anesthetic to remove any remaining pieces.
- See 3.4, CONJUNCTIVAL LACERATION if there is a significant conjunctival laceration.
- A topical antibiotic (e.g., bacitracin ointment, trimethoprim/polymyxin B drops, or fluoroquinolone drops q.i.d.) may be used.
- Preservative-free artificial tears may be given as needed for irritation.
Follow Up
- Corneal foreign body: Follow up as with corneal abrasion (see 3.2, CORNEAL ABRASION). If residual rust ring remains, reevaluate in 24 hours.
- Conjunctival foreign body: Follow up as needed, or in 1 week if residual foreign bodies were left in the conjunctiva.