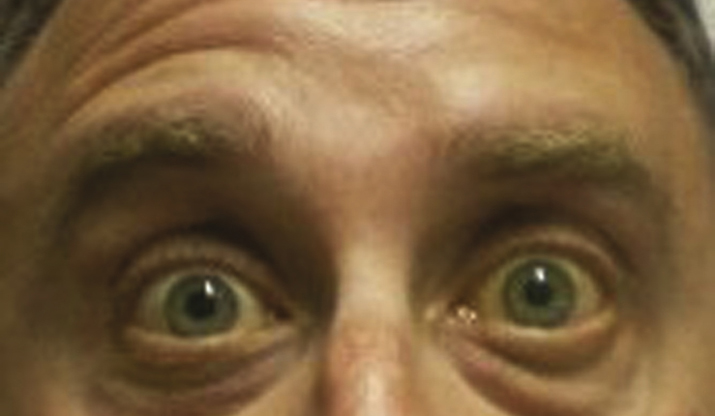
(See Figures 10.9.1 and 10.9.2.)
Critical
Unilateral weakness or paralysis of the facial musculature.
- Central lesion: Weakness or paralysis of lower facial musculature only. Upper eyelid closure and forehead wrinkling intact.
- Peripheral lesion: Weakness or paralysis of upper and lower facial musculature.
Other
Flattened nasolabial fold, droop of corner of the mouth, ectropion, and lagophthalmos. May have ipsilateral decreased taste on anterior two-thirds of tongue, decreased basic tear production, or hyperacusis. May have an injected eye with a corneal epithelial defect. Synkinesis, a simultaneous movement of muscles supplied by different branches of the facial nerve or simultaneous stimulation of visceral efferent fibers of facial nerve (e.g., corner of mouth contracts when eye closes, excessive lacrimation when eating [“crocodile” tears]), secondary to aberrant regeneration implying chronicity.