After 5 years of medication use (sooner in presence of major risk factors), begin annual screening:
- Automated visual fields: Preferably white SITA testing and 10-2 pattern for non-Asians. 24-2 or 30-2 pattern recommended for Asian patients in whom toxicity often manifests in the more peripheral macula.
- Spectral domain OCT: Parafoveal photoreceptor layer thinning and/or disruption of outer retinal layers (“flying saucer sign”), RPE atrophy, loss of foveal contour. Consider wide angle scans including vascular arcades in Asian patients.
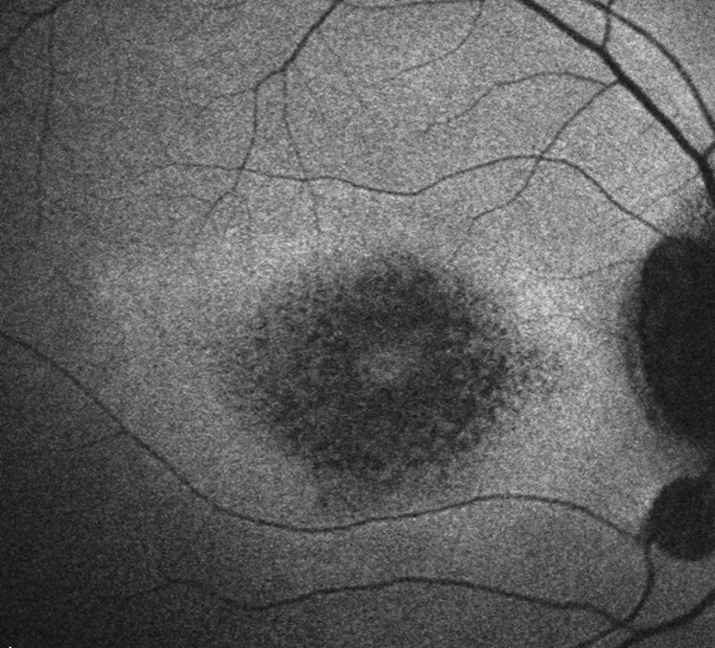
- Additional tools that may be used as available or in suspect cases include multifocal ERG and FAF (see Figure 11.32.1)
Once ocular toxicity develops, it usually does not regress even if the drug is withdrawn. In fact, new toxic effects may develop, and old ones may progress even after the chloroquine/hydroxychloroquine has been discontinued. |