Gradual loss of central vision, Amsler grid changes; may be asymptomatic.
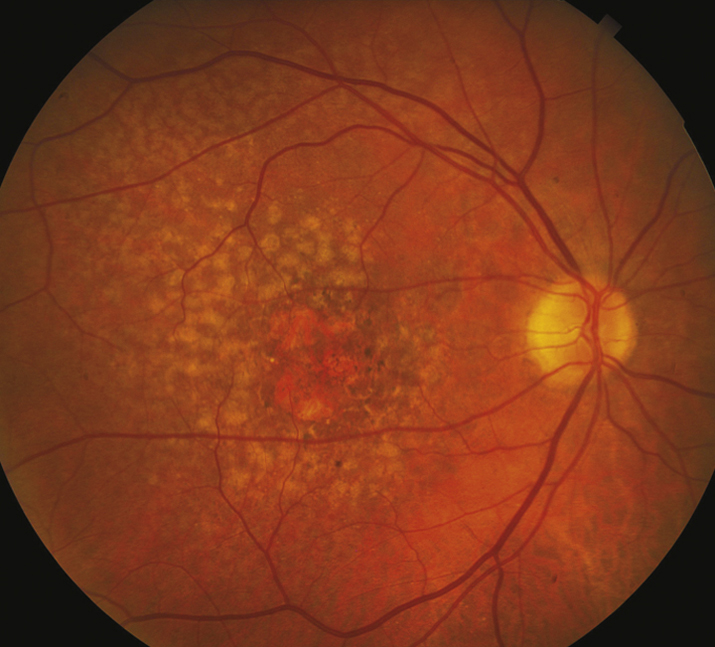
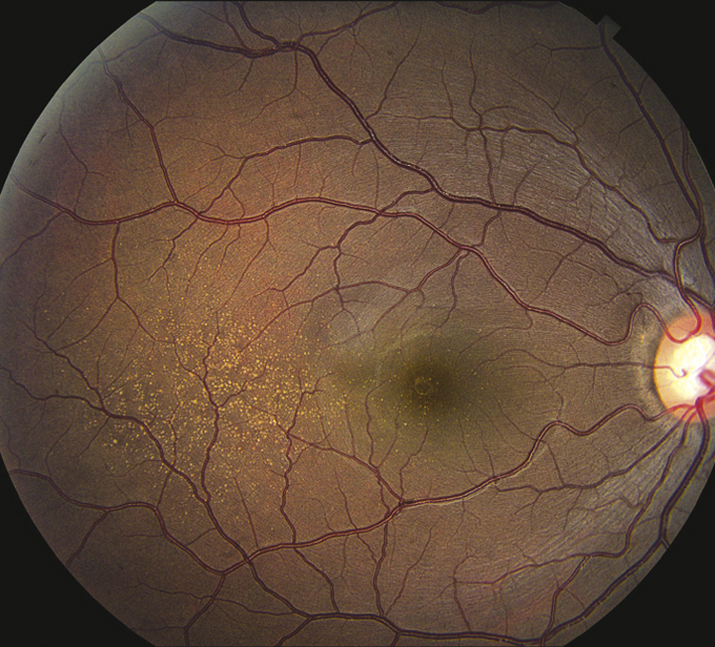
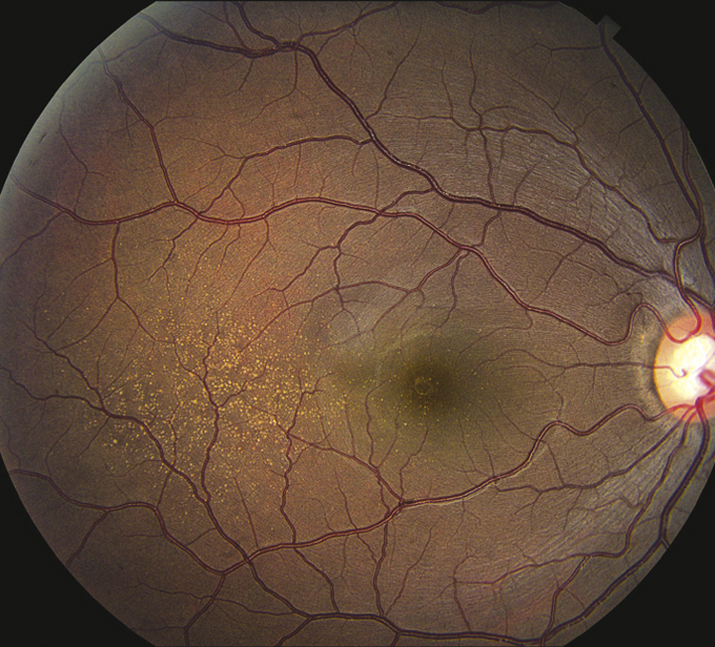
(See Figures 11.16.1 and 11.16.2.)
Critical
Macular drusen, clumps of pigment in the outer retina, and RPE atrophy, almost always in both eyes.
Other
Confluent retinal and choriocapillaris atrophy (e.g., geographic atrophy), dystrophic calcification.
11-16.2 Dry AMD with soft drusen.
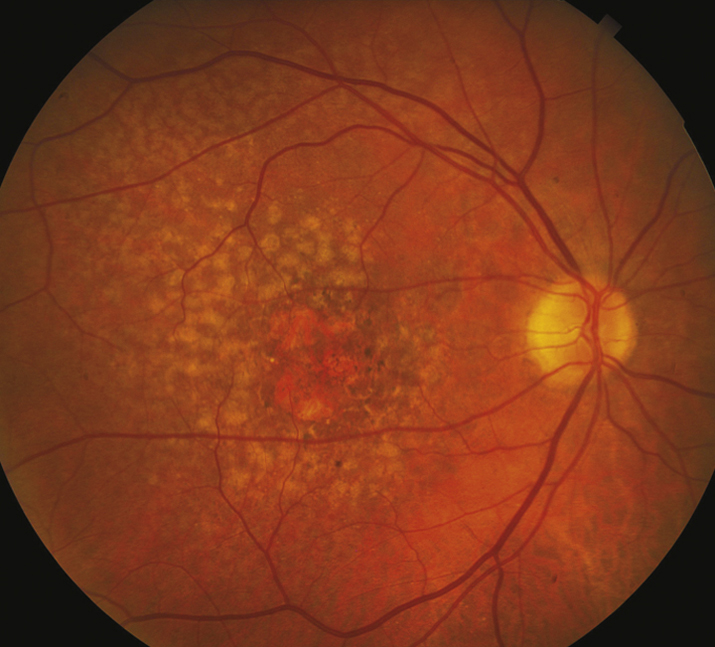
11-16.1 Dry AMD with fine drusen.
Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta-carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001;119:1417-1436.The Age-Related Eye Disease Study 2 (AREDS2) Research Group. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: The age-related eye disease study 2 (AREDS2) randomized clinical trial. J Am Med Assoc. 2013;309(19):2005-2015.AREDS2-HOME Study Research Group; Chew EY, Clemons TE, et al. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the Eye (HOME) study. AREDS2-HOME Study. Ophthalmology. 2014;121(2):535-544.
Patients with intermediate dry AMD (one large druse [125 microns] and/or ≥20 medium drusen [63 to 125 microns]), or advanced dry or exudative AMD in one eye but not the other eye, are at high risk for development of advanced stages of AMD. The original Age-Related Eye Disease Study (AREDS) report demonstrated that treatment with a vitamin/mineral formula consisting of vitamin C (500 mg), vitamin E (400 IU), beta-carotene (15 mg), zinc (80 mg), and cupric oxide (5 mg) reduces the risk of progression to advanced AMD by approximately 25% over 5 years and reduces the risk of vision loss caused by advanced AMD by approximately 19% by 5 years. A second study (AREDS2) evaluated the role of increased intake of different carotenoids (lutein and zeaxanthin) as well as two specific omega-3 long-chain polyunsaturated fatty acids (docosahexaenoic acid [DHA] + eicosapentaenoic acid [EPA]). The addition of lutein + zeaxanthin, DHA + EPA, or both to the original AREDS formulation did not further reduce risk of progression to advanced AMD but was found to be equally effective.
 NOTE: NOTE: |
Beta-carotene (in the original AREDS formula) should be withheld in past or present smokers because of increased risk of lung cancer. The AREDS2 formulation (with lutein + zeaxanthin) is preferred as it does not contain beta-carotene. |
In addition, recommend consumption of green leafy vegetables if approved by a primary care physician (intake of vitamin K decreases effectiveness of warfarin) and foods containing high levels of omega-3 fatty acids such as cold water fish and nuts.
- Low-vision aids may benefit some patients with bilateral loss of macular function.
- Refer to an internist for management of presumed risk factors: HTN, hypercholesterolemia, smoking cessation, etc.
- Those at high risk for progressing to exudative AMD may benefit from home monitoring technology for earlier detection such as the PHP ForseeHome device. Early detection of CNV increases the likelihood of better visual acuity results after intravitreal anti-VEGF therapy is initiated.
- Certain genetic mutations confer an increased risk for AMD (e.g., polymorphisms of complement factor H and ARMS2 genes). This may or may not influence response to treatment and so, at this time, genetic screening in AMD patients is not routinely performed.
Every 6 to 12 months, watching for signs of the exudative form. Daily use of Amsler grid or PHP device with instructions to return promptly if a change is noted.