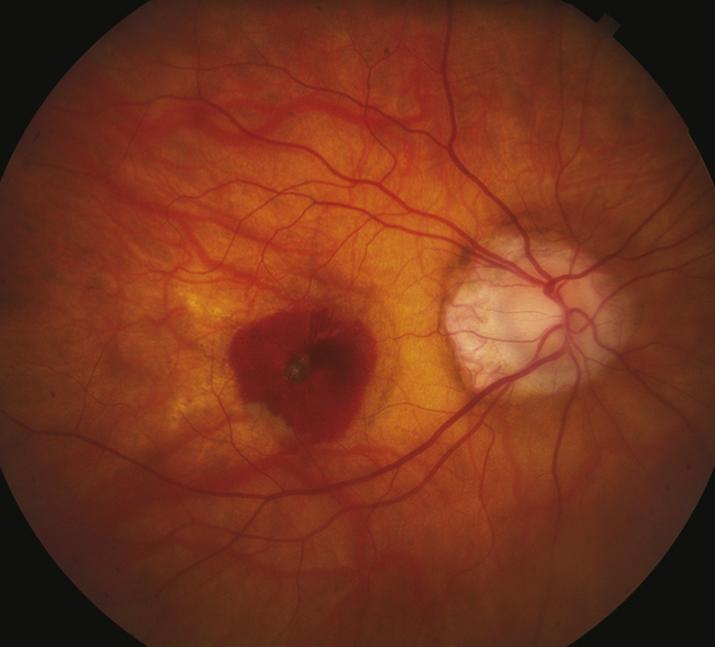
(See Figure 11.22.1.)
Critical
Myopic crescent (a crescent-shaped area of white sclera or choroidal vessels adjacent to the disc, separated from the normal-appearing fundus by a hyperpigmented line); an oblique (tilted) insertion of the optic disc, with or without vertical elongation. Macular pigmentary abnormalities; hyperpigmented spots in the macula (Fuchs spots). Typically, a refractive correction of more than −6.00 diopters, axial length ≥26.5 mm.
Other
Risk for CNV or RRD. Temporal optic disc pallor, posterior staphyloma, entrance of the retinal vessels into the nasal part of the optic cup. The retina and choroid may be seen to extend over the nasal border of the optic disc. Well-circumscribed areas of atrophy, spots of subretinal hemorrhage, choroidal sclerosis, yellow subretinal streaks (lacquer cracks), peripheral retinal thinning, and lattice degeneration may occur. Visual field defects may be present.