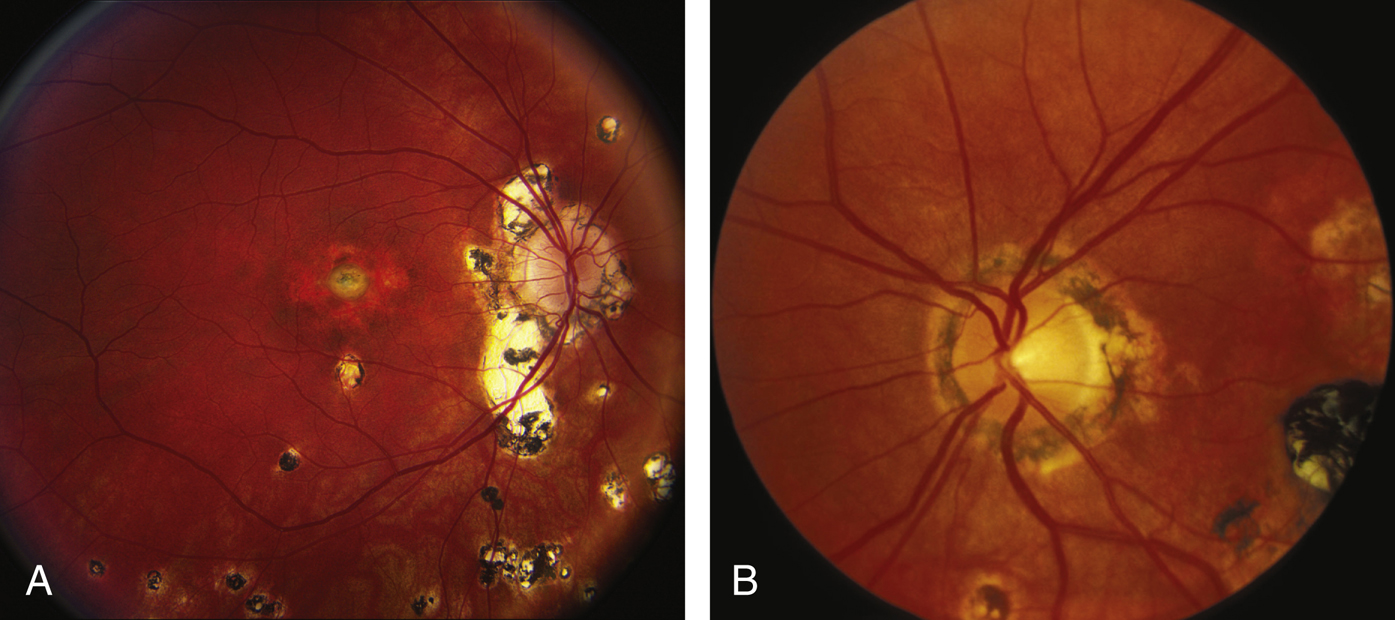
(See Figure 11.24.1.)
Critical
Classic triad. Need two of the three to make the diagnosis:
- Yellow-white, punched-out round spots, chorioretinal scars, usually <1 mm in diameter in any fundus location (histo-spots). Pigment clumps in or at the margin of the spots may be seen.
- A macular CNV appearing as a gray-green patch beneath the retina, associated with retinal edema, SRF, subretinal blood or exudate, or a pigment ring evolving into a disciform scar.
- Peripapillary atrophy or scarring, sometimes with nodules or hemorrhage. There may be a rim of pigment separating the disc from the area of atrophy or scarring.
Other
Curvilinear rows of small histo-spots in the peripheral fundus. No vitreous or aqueous cells.