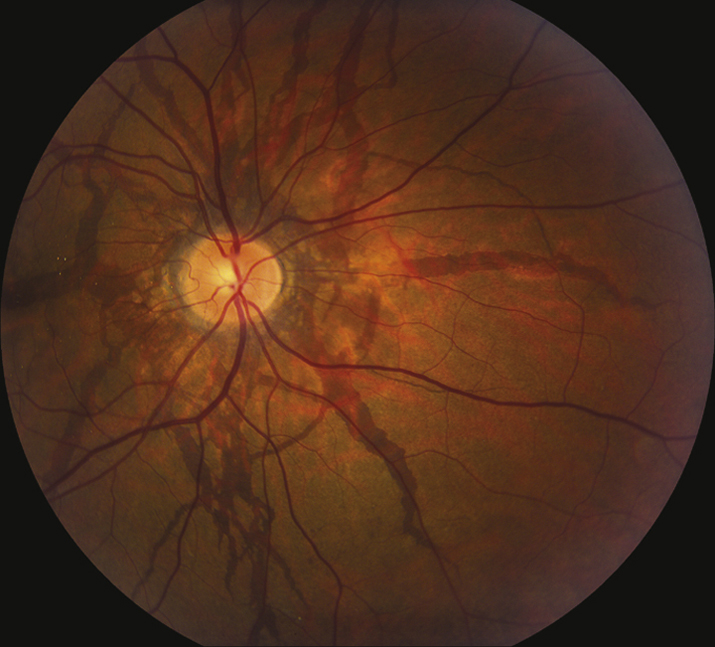
(See Figure 11.23.1.)
Critical
Bilateral reddish-brown or gray bands located deep to the retina, due to breaks within Bruch membrane, usually radiating in an irregular or spoke-like pattern from the optic disc. CNV may occur.
Other
Mottled fundus appearance with an orange hue (peau d’orange), most common in the temporal midperiphery. Subretinal hemorrhages after mild blunt trauma. Reticular pigmentary changes in the macula; small, white, pinpoint chorioretinal scars (histo-like spots) in the midperiphery; crystalline bodies within the macula. Drusen of the optic disc (especially with pseudoxanthoma elasticum [PXE]). Granular pattern of hyperfluorescent lines on IVFA. Widespread RPE damage is more evident on FAF compared to fundus ophthalmoscopy or IVFA.