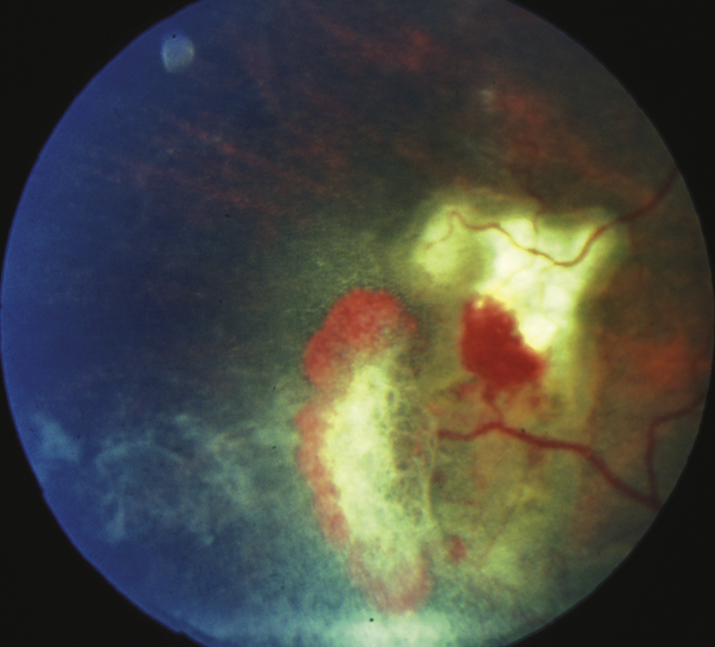
(See Figure 11.20.1.)
Critical
Peripheral retinal neovascularization in the shape of a fan (“sea fan sign”), sclerosed peripheral retinal vessels, or a dull gray peripheral fundus background color as a result of peripheral arteriolar occlusions and ischemia.
Other
Venous tortuosity, midperipheral fundus pigmented lesions with spiculated borders (black sunbursts), superficial intraretinal hemorrhages (salmon patch), refractile (iridescent) intraretinal deposits following hemorrhage resorption, angioid streaks, comma-shaped capillaries of the conjunctiva (especially along the inferior fornix). VH and traction bands, RD, CRAO, macular arteriolar occlusions, and enlargement of the foveal avascular zone occasionally develop.
Staging
- Stage 1: Peripheral arteriolar occlusions.
- Stage 2: Peripheral arteriovenous anastomoses.
- Stage 3: Neovascular proliferation.
- Stage 4: VH.
- Stage 5: RD.