Blurred vision and floaters. Scotomas and metamorphopsia are common. Photopsias are often present in posterior uveitis. Pain, redness, and photophobia are often present due to anterior chamber inflammation.
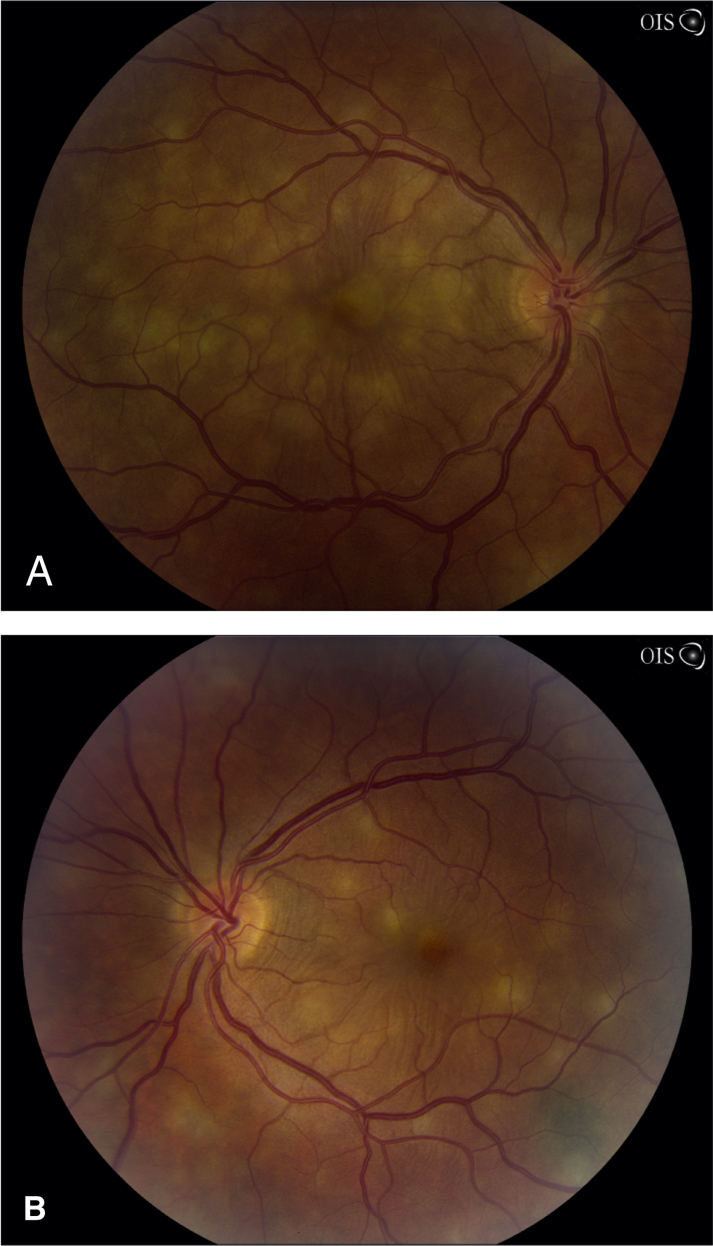
Panuveitis describes a pattern of severe, diffuse inflammation of both anterior and posterior segments. Often bilateral. Endophthalmitis or posterior scleritis should be considered in patients with posterior uveitis and significant pain. |