Salzmann nodular degeneration is a fairly common, unilateral or bilateral condition characterized by smooth creamy-white elevated lesions of the cornea. Found much more commonly in women.
Often asymptomatic. May affect vision if it involves the paracentral or central cornea. It may cause a foreign-body sensation if the lesions become very elevated.
Critical
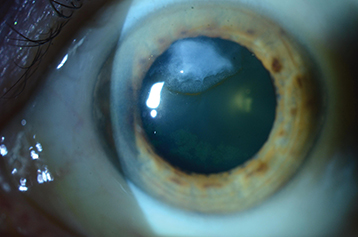
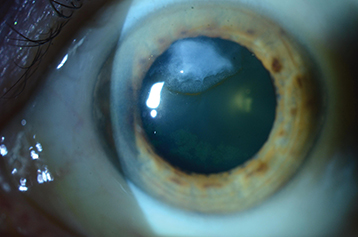
Single or multiple, discrete, white or gray-white or occasionally bluish, smooth, elevated nodules on the surface of the cornea, typically peripheral but can be central (see Figure 4.10.1).
Figure 4.10.1: Salzmann nodular degeneration with an iron line.
Other
Long-standing nodules may have iron pigment deposition in the epithelium at the base of the nodule. Corneal topography can reveal significant central irregular astigmatism from fairly mild and peripheral nodules.
A subepithelial deposition of disorganized extracellular matrix from unknown cause. It is often found in eyes with a history of chronic keratopathy, such as interstitial keratitis (IK), vernal keratoconjunctivitis, dry eye syndrome, phlyctenulosis, and trachoma, and in eyes with a history of chronic contact lens wear, trauma or corneal surgery, but frequently appears in otherwise normal eyes.
Asymptomatic patients can be checked every 1 to 2 years. Symptomatic patients should be seen more frequently. Nodules should be measured at follow-up visits to look for progression. Consider checking corneal topography routinely to monitor the degree of irregular astigmatism.