Usually asymptomatic, although patients with advanced disease may present with decreased vision or visual field loss. Intermittent eye pain, headaches, and blurry vision may occur.
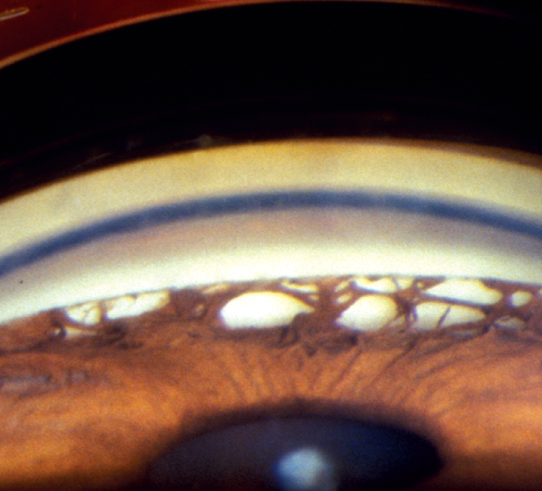
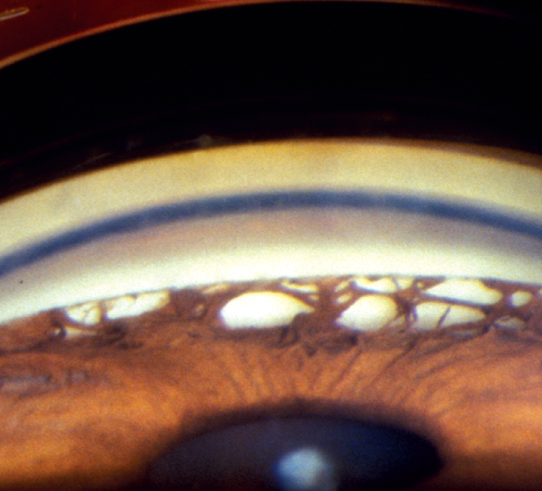
(See Figure 9.5.1.)
Figure 9.5.1: Chronic angle closure glaucoma with peripheral anterior synechiae.
Critical
Gonioscopy reveals broad bands of PAS in the angle in most patients. In some patients there is no PAS, despite having iridotrabecular contact on indentation gonioscopy. The PAS block visualization of the underlying angle structures. Glaucomatous optic nerve and visual field defects.
Other
Elevated IOP.
Gradual narrowing of the angle with prolonged appositional closure.
Prolonged acute angle-closure glaucoma or multiple episodes of subclinical attacks of acute angle closure.
Previous flat anterior chamber from surgery, trauma, or hypotony that resulted in the development of PAS.
PAS secondary to the chronic uveitis, regressed neovascular glaucoma.
|
 NOTE NOTEWhile acute angle closure is less common in those of African descent, chronic angle closure is more common in these patients. |
See 9.1, Primary Open-Angle Glaucoma.
LT is contraindicated in CACG and can induce greater scarring of the angle.
Laser iridotomy is indicated to relieve any component of pupillary block and to prevent ongoing development of PAS if closure is not already 360 degrees. Beware of post-laser IOP spikes in these patients whose TM function may be limited.
Laser iridoplasty may be performed (and repeated) to decrease the formation of new PAS in those without 360 degrees of PAS. This may not be entirely effective and may serve only as a temporizing measure. If iridoplasty fails and other medical therapy has been maximized, the patient may need surgical intervention. Endoscopic cyclophotocoagulation (ECP) may be attempted in cases with early glaucoma, but trabeculectomy or tube shunt is usually indicated in more advanced cases in addition to removing the cataract. MIGS is usually contraindicated due to closed angle. If intraoperative gonioscopy after cataract extraction shows an open angle, some MIGS such as goniotomy could be considered in mild to moderate cases.
See 9.1, Primary Open-Angle Glaucoma.