FEVR: Can appear similar to ROP, except FEVR is hereditary (although family members may be asymptomatic, and de novo mutations frequently occur) and more often asymmetric; asymptomatic family members often show peripheral retinal vascular abnormalities. There usually is no history of prematurity or oxygen therapy. See 8.3, Familial Exudative Vitreoretinopathy.
Incontinentia pigmenti: X-linked dominant condition that usually occurs in girls. Often lethal in males. Characterized by skin changes including erythematous maculopapular lesions, vesicles, hypopigmented patches, and alopecia. Associated with eosinophilia. Central nervous system (CNS) and dental abnormalities also seen.
See 8.1, Leukocoria, for additional differential diagnoses.
Classification
Zone I: Posterior pole: Twice the disc–fovea distance, centered around the disc (poorest prognosis).
Zone II: From zone I to the nasal ora serrata; temporally equidistant from the disc.
Number of clock hours (30-degree sectors) involved. Of note, the number of clock hours of neovascularization was important in older treatment criteria, but it is not used in the most updated treatment guidelines.
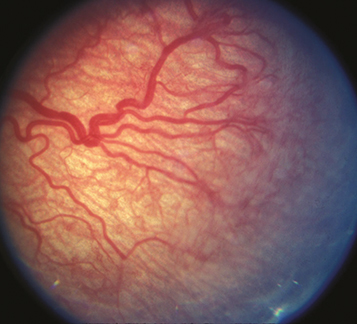
Stage 1: Flat demarcation line separating the vascular posterior retina from the avascular peripheral retina (see Figure 8.2.1).
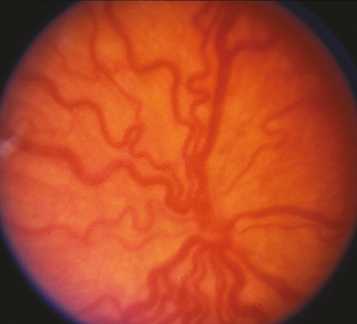
Stage 3: Ridged demarcation line with fibrovascular proliferation or neovascularization extending from the ridge (see Figure 8.2.2).
Overall stage is determined by the most severe manifestation; however, it is recommended to define each stage and extent. |
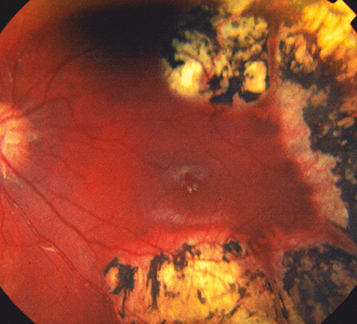
Posterior pole engorgement and tortuosity of veins and arteries; iris vascular engorgement, poor pupil dilatation, and vitreous haze with more advanced plus disease. If plus disease is present, a “+” is placed after the stage (e.g., stage 3+). If vascular dilatation and tortuosity are present but inadequate to diagnose plus disease, it is called “pre-plus” disease and noted after the stage (e.g., stage 3 with pre-plus disease). “Aggressive ROP,” rapidly progressing posterior ROP with extensive plus disease, formerly known as “rush” disease, may progress rapidly to stage 5 ROP without passing through the other stages. This aggressive ROP may also show hemorrhages at the junction between vascular and avascular retina (see Figure 8.2.3).
Defines high-risk eyes that meet the criteria for treatment:
Defines less severely advanced eyes that should be monitored closely for progression to type 1 disease:
Screening Recommendations
Selected infants with birth weight >1,500 g or gestational age ≥31 weeks with unstable clinical course thought to be at high risk.
Timing of first eye examination is based on postmenstrual (gestational age at birth plus chronologic age) and postnatal (chronologic since birth) age. The first eye examination should start at 31 to 32 weeks postmenstrual age or 4 weeks postnatal age, whichever is later.
The American Academy of Pediatrics provides updated guidelines for ROP screening in premature infants. For the latest recommendations, please see their most recent policy statement available at aap.org. |