Decreased vision, floaters, and pain that is often bilateral. Patients typically have a history of recent hospitalization, recent abdominal surgery, being immunocompromised, possessing a long-term indwelling line or catheter (e.g., for hyperalimentation, hemodialysis, or antibiotics), or using intravenous drugs.
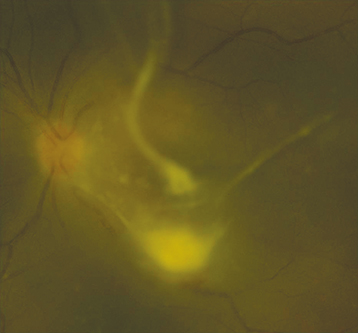
(See Figure 12.18.1.)
Figure 12.18.1: Candida chorioretinitis with vitreous involvement.
Critical
Discrete, multifocal, yellow-white, choroidal to chorioretinal fluffy lesions from one to several disc diameters in size. With time, the lesions increase in size, break into the vitreous, and appear as a “string of pearls,” especially in the case of Candida. Aspergillus has a predisposition for the subretinal space.
Other
Vitreous cell and haze, vitreous abscesses, retinal hemorrhages with or without pale centers, AC cells, and hypopyon. A retinal detachment may develop.
The following should be considered in immunocompromised patients.
CMV retinitis: Multifocal areas of granular retinal whitening with a minimal to mild vitreous reaction, more likely to be associated with retinal hemorrhage. See 12.12, Cytomegalovirus Retinitis.
Toxoplasmosis: Yellow-white retinal lesions often with an adjacent chorioretinal scar. See 12.9, Toxoplasmosis.
Pneumocystis choroidopathy: Rare manifestation of widely disseminated Pneumocystis carinii infection. Usually in AIDS patients. Often asymptomatic. History of P. carinii and treatment with aerosolized pentamidine. Multifocal, yellow, round, deep choroidal lesions approximately one-half to two-disc diameters in size, located in the posterior pole. No vitritis. Patients are often cachectic. Treatment is with i.v. trimethoprim/sulfamethoxazole or i.v. pentamidine in conjunction with an infectious disease specialist.
Others: Herpes viral retinitis; Nocardia, and Cryptococcus species; atypical Mycobacterium, coccidioidomycosis, and others.