Blurred vision and floaters. May have redness and photophobia. Pain depends on the severity of associated iridocyclitis.
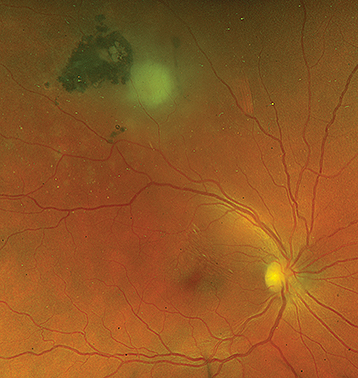
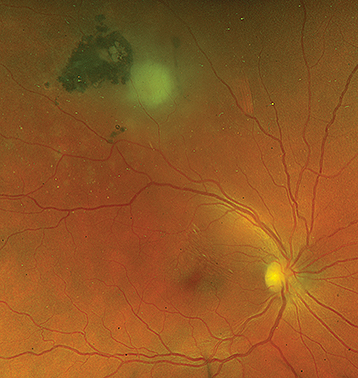
(See Figure 12.9.1.)
Figure 12.9.1: Area of active toxoplasmosis retinochoroiditis adjacent to a pigmented scar.
Critical
New, unilateral “fluffy” white retinal lesion often associated with an old pigmented chorioretinal scar. There is a moderate to severe focal vitreous inflammatory reaction directly over the lesion, which may obscure the active lesion on dilated fundus examination, resulting in the “headlight-in-fog” sign. Scar may be absent in cases of newly acquired toxoplasmosis or in immunocompromised patients.
Other
Anterior: Mild AC spillover may be present, with increased IOP in 10% to 20%.
Posterior: Vitreous debris, optic disc swelling due to peripapillary lesions often with edema extending into the retina, neuroretinitis with/without macular star, optic neuritis with significant vitritis, retinal vasculitis, rarely retinal artery or vein occlusion in the area of the inflammation. Kyrieleis plaques are periarterial exudates, which may occur near the retinitis or elsewhere in the retina; IVFA typically does not show vascular occlusion. Chorioretinal scars are occasionally found in the uninvolved eye. CME, retinal neovascularization and retinal detachment may also be present.
See 12.3, Posterior Uveitis, for a complete list. The following rarely may closely simulate toxoplasmosis.
Syphilis (see 12.10, Syphilis) and TB.
Toxocariasis: Usually affects children. Chorioretinal scars are not typically seen. See 12.4, Panuveitis and 8.1, Leukocoria.
ARN. See 12.13, Acute Retinal Necrosis(see Table 12.12.1).
PORN. See 12.13, Acute Retinal Necrosis(see Table 12.12.1).
|
 NOTE NOTEToxoplasmosis is the most common cause of posterior uveitis and accounts for approximately 90% of focal necrotizing retinitis. Infection can be congenital or acquired. |
See 12.4, Panuveitis, for workup recommendations when the diagnosis is in doubt.
History: risk factors include handling or eating raw meat (e.g., venison), exposure to cats or especially kittens (sources of acquired infection), and hunters who dress their own game. Inquire about risk factors for HIV in atypical cases (e.g., multifocal retinitis). Water- and air-borne outbreaks of toxoplasmosis have been reported.
Complete ocular examination, including an IOP check and a dilated fundus examination.
Focused serologic testing based on history and examination:
Serum anti-Toxoplasma antibody titer to indicate remote (IgG) or recent (IgM) infection (usually not necessary). IgM is found approximately 2 weeks to 6 months after initial infection, after which only IgG remains positive.
|
 NOTE NOTEA negative toxoplasmosis serum antibody titer (IgG and IgM) makes the diagnosis of toxoplasmosis highly unlikely. |
Treponemal test (syphilis EIA, FTA-ABS, TP-PA), followed by confirmatory nontreponemal test (RPR, VDRL). See 12.10, Syphilis.
Interferon gamma releasing assay (IGRA, QuantiFERON Gold) and/or PPD. Consider chest imaging (CXR or CT chest) to assess for signs of active or prior pulmonary disease.
In those at risk for TB (e.g., immigrants from high-risk areas such as India, HIV-positive patients), homeless patients, or prisoners.
If considering immunosuppressive therapy (especially biologics).
ACE, lysozyme, and chest imaging (CXR or CT chest).
PCR testing from aqueous or vitreous specimens for Toxoplasma gondii is more specific than serologic testing.
Ocular fluid for PCR testing for Toxoplasma DNA may be acquired through AC or vitreous taps or via diagnostic vitrectomy in equivocal cases.
Consider HIV testing in atypical cases or high-risk patients. See below.
Initially, every 3 to 7 days to ensure improvement, then every 1 to 4 weeks while on therapy.
SPECIAL CONSIDERATION IN IMMUNOCOMPROMISED PATIENTS
Vitritis is usually much less prominent. Adjacent retinochoroidal scars may not be present. The lesions may be single or multifocal, discrete or diffuse, and unilateral or bilateral. CNS imaging is essential because of high association with CNS disease (e.g., toxoplasmic encephalitis in HIV patients). Diagnostic vitrectomy may be necessary because of the multiple simulating entities and the variability of laboratory diagnostic tests. Systemic steroids for ocular toxoplasmosis should be used very cautiously in patients with AIDS.