ACQUIRED SYPHILIS
Most patients with syphilis will never develop ocular involvement. A history of sexually transmitted disease, HIV, or high-risk sexual activity should be elucidated. Men who have sex with men are at an increased risk, but heterosexual transmission is on the rise.
Primary: Chancre (ulcerated, painless lesion), regional lymphadenopathy.
Secondary: Skin or mucous membrane lesions, generalized lymphadenopathy, constitutional symptoms (e.g., sore throat, fever), and symptomatic or asymptomatic meningitis.
Tertiary: Cardiovascular disease (e.g., aortitis), CNS disease (e.g., meningovascular disease, general paresis, and tabes dorsalis).
Primary: A chancre may occur on the eyelid or conjunctiva, madarosis (loss of lashes or eyebrows).
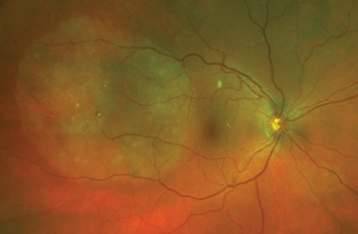
Secondary: Uveitis (posterior and panuveitis more common than anterior), optic neuritis, chorioretinitis, serous retinal detachments, retinitis, retinal vasculitis, conjunctivitis, dacryoadenitis, dacryocystitis, episcleritis, scleritis, interstitial keratitis, and others. See Figure 12.10.1.
Tertiary: Optic atrophy, old chorioretinitis, interstitial keratitis, chronic uveitis, Argyll Robertson pupil (see 10.3, Argyll Robertson Pupils), in addition to signs seen in secondary disease.
See 12.1, Anterior Uveitis (Iritis/Iridocyclitis), 12.2, Intermediate Uveitis, 12.3, Posterior Uveitis, and 12.4, Panuveitis, for anatomic location-specific differential diagnoses.
See 12.1, Anterior Uveitis (Iritis/Iridocyclitis), 12.2, Intermediate Uveitis, 12.3, Posterior Uveitis, and 12.4, Panuveitis, for anatomic location-specific uveitis workup recommendations.
Complete ophthalmic examination, including pupillary and dilated fundus examination. Palmar skin lesions are common and easily assessed in the clinic.
The “reverse algorithm” should be used, with treponemal testing done first to confirm the disease, and (if reactive) then nontreponemal testing is performed to monitor for treatment response. Treponemal testing with EIA, chemiluminescent immunoassays (CIA), FTA-ABS, or T. pallidum microhemagglutination assay (MHA-TP) tests are highly sensitive and specific in all but the primary stage of syphilis, during which ocular involvement is very rare. Once reactive, treponemal tests do not normalize and cannot be used to assess the patient’s response to treatment. Quantitative nontreponemal tests such as RPR or VDRL are then done to assess the activity of the infection and are then repeated periodically after treatment to confirm resolution of infection.
VDRL and RPR should not be used for screening as false-negative results can occur in early primary, latent, or late syphilis due to low sensitivity. False-negative results are also possible due to interference from excessively high titers (prozone reaction). False-positive results can occur due to viral illnesses, pregnancy, and test cross-reactivity with autoimmune or collagen vascular diseases. RPR and VDRL titers are used to follow treatment response.
HIV testing is indicated in any patient with syphilis because of the relatively aggressive course in HIV-coinfected individuals as well as the high frequency of co-infection.
Patients should be evaluated for concomitant sexually transmitted diseases, with notification sent to the local health department when indicated.
Consider lumbar puncture with VDRL or FTA-ABS testing, protein, and cell count with differential in cases of confirmed syphilitic uveitis to assess for comorbid neurosyphilis. Persistently stable or elevated CSF VDRL titers are concerning for incomplete treatment or reinfection.
In the presence of uveitis consistent with syphilis:
Treponemal testing negative: Syphilis unlikely, consider retesting if there is high suspicion and/or evaluating for other causes of uveitis.
Treponemal testing positive and nontreponemal testing negative:
Treponemal testing positive and nontreponemal testing positive: Treat for syphilis.
Syphilitic uveitis represents a breakdown of the blood–brain (ocular) barrier and should be treated as neurosyphilis with: penicillin G 3 to 4 million units q4h for 14 days.
If anterior segment inflammation is present, treatment with a cycloplegic (e.g., cyclopentolate 1% b.i.d.) and topical steroid (e.g., prednisolone acetate 1% q2h) should be started.
Oral steroids may be started 24 to 48 hours after induction of penicillin therapy and may speed visual recovery, but ultimately, have not been shown to affect final visual outcomes. Oral steroids may also help prevent systemic inflammatory complications associated with the Jarisch–Herxheimer reaction.
Uveitis (negative CSF VDRL): Repeat serum VDRL/RPR testing q3 months after treatment. If a titer of 1:8 or more does not decline fourfold within 6 months, the titer increases fourfold, or clinical symptoms or signs of syphilis persist or recur, then repeat lumbar puncture checking VDRL and retreatment may be indicated. If a pretreatment VDRL/RPR titer is <1:8, retreatment is indicated only when the titer increases or when signs of syphilis recur.
Uveitis and neurosyphilis (positive CSF VDRL): Requires follow-up with an infectious disease specialist. Repeat lumbar puncture should be performed every 6 months for 2 years, less frequently if the cell count returns to normal sooner. The cell count should decrease to a normal level within this period, and the CSF VDRL titer should decrease fourfold within 6 to 12 months. A significantly elevated CSF protein decreases more slowly. Failure of these indices to improve is concerning for incomplete treatment or reinfection.