Painless floaters and blurred vision. Minimal photophobia or complaints of external inflammation (e.g., red eye). Most often is bilateral (but can be unilateral or very asymmetric) and most frequently affects patients aged 15 to 40 years.
Critical
Vitreous cells and cellular aggregates float predominantly in the inferior vitreous (“snowballs”). Younger patients may present with vitreous hemorrhage. White exudative material over the inferior ora serrata and pars plana (“snowbank”) is suggestive of pars planitis.
|
 NOTE NOTESnowbanking is typically located in the inferior vitreous and can often be seen only with indirect ophthalmoscopy and scleral depression. |
Other
Peripheral retinal vascular sheathing, peripheral neovascularization, mild AC inflammation, CME, posterior subcapsular cataract, band keratopathy, secondary glaucoma, ERM, peripheral retinal cysts, and tractional retinal detachments. Posterior synechiae in pars planitis are uncommon and, if present, usually occur early in the course of the disease. Choroidal neovascularization (CNV) is rare.
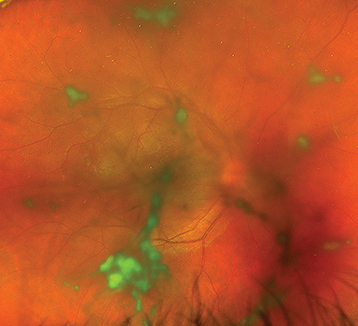
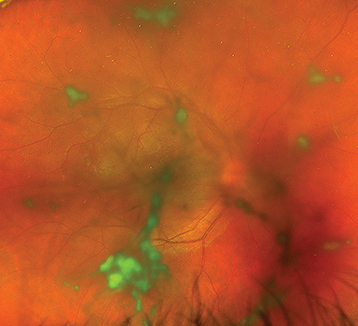
(See Figure 12.2.1.)
Figure 12.2.1: Clumps of snowballs in the anterior vitreous of a young boy with pars planitis.
Diagnostic Categories
Bartonella
IBD-associated intermediate uveitis
JIA-associated intermediate uveitis (in children)
Multiple sclerosis (MS)–associated intermediate uveitis
Pars planitis
Sarcoidosis
Syphilis
TINU
Vitreoretinal lymphoma
Mild vitreous cells in the absence of significant symptoms, CME, or vision loss may be observed in cases of noninfectious intermediate uveitis. Treat all vision-threatening complications (e.g., CME, progressive snowbanks, peripheral nonperfusion) in symptomatic patients with active disease.
Topical prednisolone acetate 1% or difluprednate 0.05% q.i.d.–q2h.
Treat infectious etiologies with appropriate antimicrobials prior to using local long-acting ocular steroids or systemic steroids.
Consider a trial of oral steroids if bilateral and incomplete response to topical steroids.
|
 NOTE NOTEIn bilateral cases, systemic steroid therapy may be preferred to periocular injections. However, in children and adolescents, growth suppression (in addition to the usual complications of long-term systemic steroids) is a major concern. |
Consider local steroid injection if unilateral or there is CME that is resistant to topical steroids.
If the disease becomes persistent, consider long-acting local steroids (0.19 mg or 0.59 mg fluocinolone acetonide implants) versus systemic steroid-sparing immunosuppression (e.g., antimetabolites, calcineurin inhibitors, and anti-TNF agents).
|
 NOTE NOTETNF-alpha inhibitors (e.g., adalimumab, infliximab) should be avoided in patients who are suspected of having MS-associated intermediate uveitis as they can precipitate or worsen demyelinating CNS disease. |
IVFA-guided panretinal photocoagulation should be considered in those with severe peripheral nonperfusion, active peripheral neovascularization, or complication from active peripheral neovascularization (e.g., vitreous hemorrhage).
|
 NOTE NOTESome physicians delay steroid injections for several weeks to observe whether the IOP increases on topical steroids (steroid response). If a marked steroid response is found, depot injections are relatively contraindicated. Intravitreal steroids are more effective for uveitic macular edema than periocular steroids. Consider adding topical NSAIDs in patients with CME, especially those who have steroid response ocular hypertension. Cataracts are a frequent complication of intermediate uveitis. If cataract extraction is performed, the patient should ideally be free of inflammation for 3 months preceding the operation. Consider starting the patient on oral prednisone 60 mg daily 2 to 5 days prior to surgery and tapering the prednisone over the next 1 to 4 weeks. Aggressive perioperative use of topical NSAIDs (e.g., ketorolac 0.5% q.i.d.) and topical steroids (e.g., prednisolone acetate 1% q2h or difluprednate 0.05% six times a day) starting 5 to 7 days preoperatively and continued for at least 4 to 6 weeks postoperatively may reduce the risk of pseudophakic CME and recurrent uveitis.
|